by Alberto J. Muniagurria and Eduardo Baravalle
EXTERNAL MALE GENITALIA
Examination of the male external genitalia can cause anxiety in the patient, as well as in female students, and even in some male students. This anxiety is a normal reaction; sometimes the patient can have an erection, and in such circumstances the doctor must finish his examination without giving importance to the fact. At other times the male patient may refuse to be examined by a female; likewise, a woman can refuse to have her pelvic exam performed by a man; In both cases, the wishes and rights of the patient must be respected, requesting help from a colleague.
The order to follow for the examination of the external genitalia is:
- External inspection of the hair, penis and scrotum.
- Palpation of regional nodes, penis, testis, epididymis and spermatic cord.
- Control of the state of the hernial orifices.
- Rectal examination, to evaluate the tone of the anal sphincter, the rectal bleb, the prostate and the presence of occult blood in fecal matter.
The genital examination is done with the patient lying down and then in the standing position, to look for hernias and the presence of a varicocele. Rubber gloves are used, and if not, manual hygiene before and after the exam is a good habit.
Inspection. Palpation
Sexual development should be evaluated, observing the characteristics of pubic hair and genitalia.
Penis. In the penis the characteristics of the skin, its shape and size are observed. The patient is asked to retract the foreskin; in case of poor hygiene, a creamy, yellowish-white material, called smegma, will be observed in the balanopreputial sulcus. The glans must be compressed to produce the opening of the urethral orifice, from which no secretion should flow.
Scrotum. The scrotal skin color and texture should be inspected, and the testicles and epididymis should also be palpated with the thumb, index, and middle finger. The shape, size, surface and consistency will be taken into account; it is normal for this palpation to produce visceral pain.
The spermatic cords will also be palpated. In order to confirm the normality of the testicles, transillumination can be used, for which, in a dark environment, a powerful light beam is directed through the scrotum. Under normal conditions the content allows transillumination.
The patient is asked to perform Valsalva maneuvers and the hernial orifices are then palpated. No protrusions or palpation of abdominal viscera in the triangle of inguinal weakness, in the superficial orifice of the inguinal canal, or in the crural orifice.
 To palpate the superficial opening of the inguinal canal, the examiner's index finger is inserted into the scrotum and, drawing the skin with the finger, palpates the external orifice of the inguinal canal, identifying the spermatic cord, the size and perimeter of the superficial ring and the Hesselbach's triangle area (Figure 11-1).
To palpate the superficial opening of the inguinal canal, the examiner's index finger is inserted into the scrotum and, drawing the skin with the finger, palpates the external orifice of the inguinal canal, identifying the spermatic cord, the size and perimeter of the superficial ring and the Hesselbach's triangle area (Figure 11-1).
Rectal examination It is an extremely useful maneuver due to the information it provides, and should never be omitted in the physical examination of men over 40 years of age. As with the genital examination, the professional attitude of the physician is very important in this examination; The objective of the maneuver must be explained to the patient and in this way he will only experience slight discomfort.
To perform the digital rectal examination, the patient must take the following positions: the position preferred by most examiners, especially for elderly or elderly people, is the left lateral decubitus, with the left leg partially flexed and the right leg frankly flexed , the left arm crossed under the chest and the right arm hanging over the table (Figure 11-2). Another position that may be useful is the knee-shoulder position, in which the patient rests both knees separately on the examining table and the left shoulder, with the left arm underneath, also leans on the table explorer; the ankles and feet extend off the table (Figure 11-3).
It can also be performed with the patient in a standing position. At the edge of the bed or gurney, the patient, in a standing position, rests his hands or elbows on the bed (Figure 11-4). The region must be well lit to properly view the anal area. Under normal conditions, the perianal skin is more pigmented.
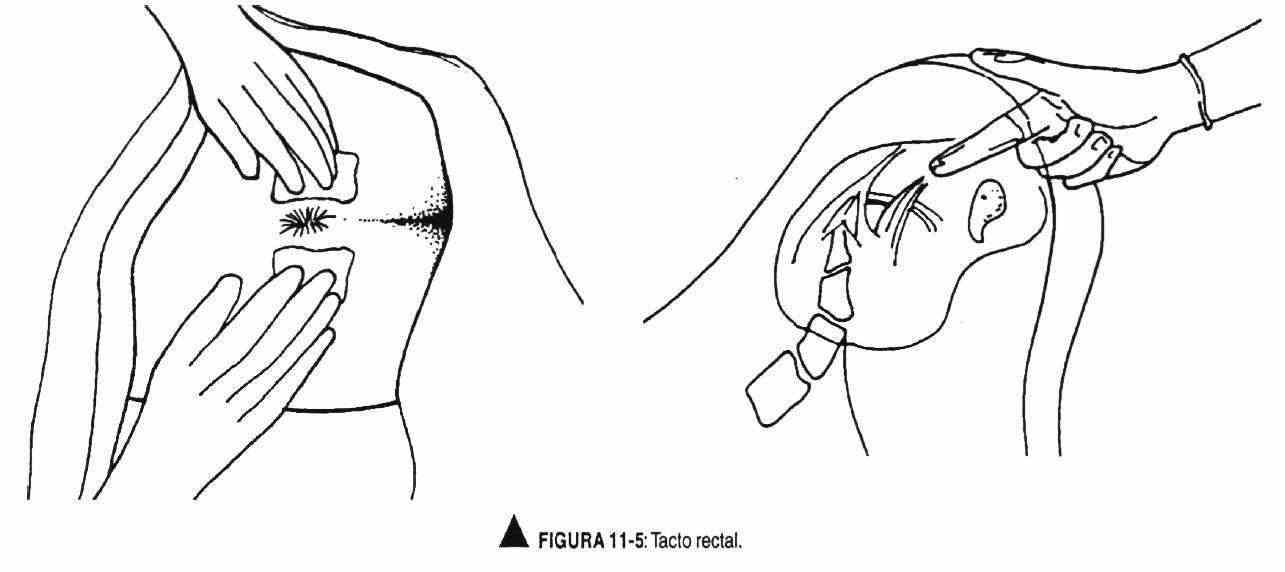
The examiner, with the gloved right hand, inserts the lubricated index finger through the anal sphincter, while the left hand separates the buttock. The anal sphincter closes around the explorer finger and begins by palpating the lateral and posterior aspects of the rectum, which should have a smooth surface and may contain fecal matter (Figure 11-5).
Then the anterior wall of the rectum is palpated to evaluate the characteristics of the prostate, its shape, lobes and median sulcus, size, limits, surface, consistency and sensitivity, taking into account that its palpation can arouse the desire to void. The examiner finger should be gently withdrawn, observing the remains of material to look for the presence of blood in the stool. The patient is offered gauze to remove excess petroleum jelly.
FEMALE GENITALS
 Examination of the female external genitalia can cause anxiety in some patients; this anxiety is a normal reaction, which the examiner should understand and conduct the examination with a professional attitude. The maneuvers to be carried out will always be explained. Each new movement must be announced in advance. This prepares the patient for the different situations that accompany the different stages of the examination. In this way you will be able to understand that the maneuvers are carried out accordingly.
Examination of the female external genitalia can cause anxiety in some patients; this anxiety is a normal reaction, which the examiner should understand and conduct the examination with a professional attitude. The maneuvers to be carried out will always be explained. Each new movement must be announced in advance. This prepares the patient for the different situations that accompany the different stages of the examination. In this way you will be able to understand that the maneuvers are carried out accordingly.
All internists, surgeons, gynecologists, and pediatricians should perform pelvic exams on their patients.
The doctor should address the patient by name, avoiding additional terms such as "grandmother", "mother", "dear", "pichona", and avoiding terms with sexual connotations.
 Thus, the term examine should be used instead of feeling or touching or palpating; say "let your knees drop to the sides" instead of "spread your legs"; and "insert" instead of "insert".
Thus, the term examine should be used instead of feeling or touching or palpating; say "let your knees drop to the sides" instead of "spread your legs"; and "insert" instead of "insert".
The opportunity will also be taken to educate the patient using lay and technical terms, trying to assess her level of knowledge to suit it. If you decide to show the speculum, you should explain how it works; otherwise its use may be misinterpreted and create fear in this part of the exam. It is necessary to accept and recognize one's own limitations and how they can affect the relationship with the patient. You should also try not to make assumptions about their degree and type of sexual activity. This attitude of the doctor can make the patient ask about her doubts. Patients usually go to the doctor in search of permissive answers. It is important to be careful, take an unambivalent attitude and not stimulate the patient beyond her own responsibility, supporting her with her emotions.
The order to be followed for the examination of the female external genitalia is:
- Examination of pubic hair
- Inspection and palpation of the vulva
- Examination in the speculum. Pap smear
- Vaginal examination
The patient should be in the supine position, with the legs apart and supported in the corresponding stirrups, with the buttocks a few centimeters outside the table. It is necessary that the patient is properly covered, and that she has previously emptied her bladder. Ideally, you should dress in a backless gown.
Before placing the patient in the proper position, it must be ensured that the necessary material is available. The light source and the bench to support a foot must be located in the corresponding place. The explorer's hands and the speculum will be at an appropriate temperature.
The speculum is an instrument that is used to open the vagina, normally closed, in order to visualize it, and also to see the cervix. Specula can be metallic or plastic; The latter, when opened, produce a metallic sound that can scare those patients who are not forewarned.
There are different sizes of specula, and the correct one must be chosen for each patient. Gloves will be disposable. At least a glove should be used on the hand that is inserted into the vagina, taking care not to touch the light source or fecal matter to avoid contamination.
At this point, the patient should be asked to drop her knees to both sides.
To avoid being startled, it is a good habit to let her know when you are going to touch her, and begin by doing it in an area outside the genital area. Care must also be taken with the vocabulary used, avoiding the use of words such as long, small, etc.
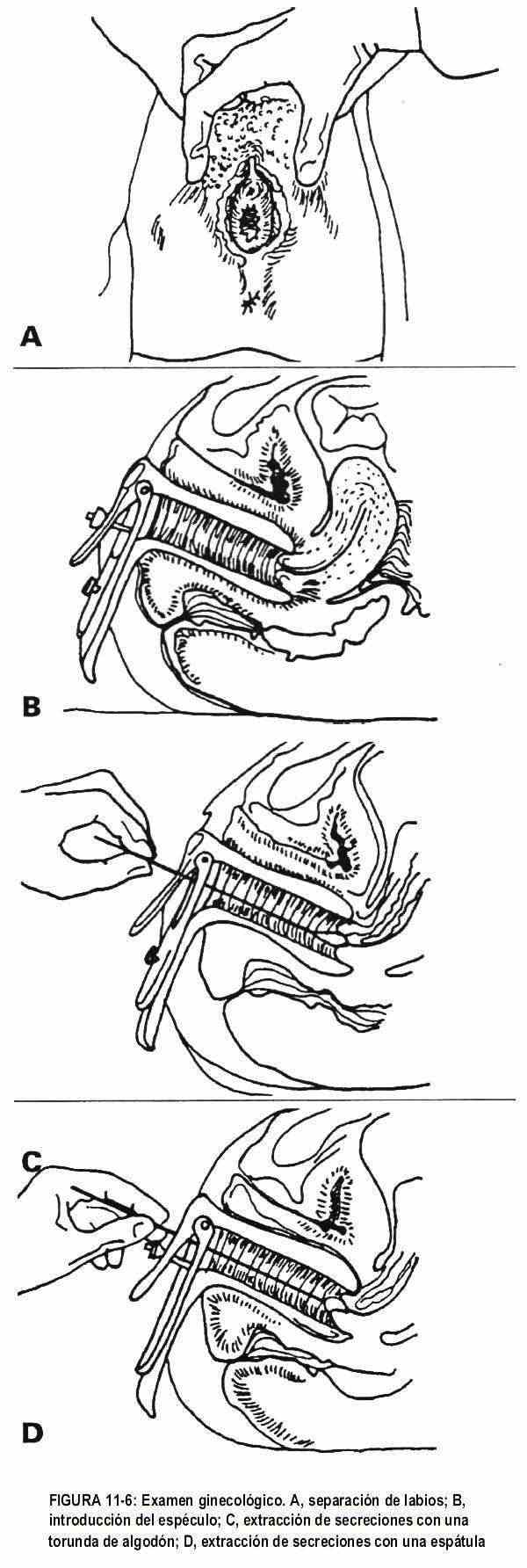
In adolescents without sexual activity, these maneuvers are not performed and only pubic hair is evaluated. The pubic hair should have a triangular shape with a superior base, varying according to the sexual development of the patient. Later, the labia majora and minora will be inspected and palpated, observing the presence or not of the hymen. The labia minora are separated and the vestibule is visualized (Figure 11-6), observing the introitus as well as the urethral meatus. To study Skene's glands, the labia minora are squeezed at 11 and 1 o'clock (considering the vulva area as included in a clock face) in order to evaluate the presence of secretion. The support of the vaginal wall should be examined; For this, the patient is asked to perform a positive Valsalva maneuver,
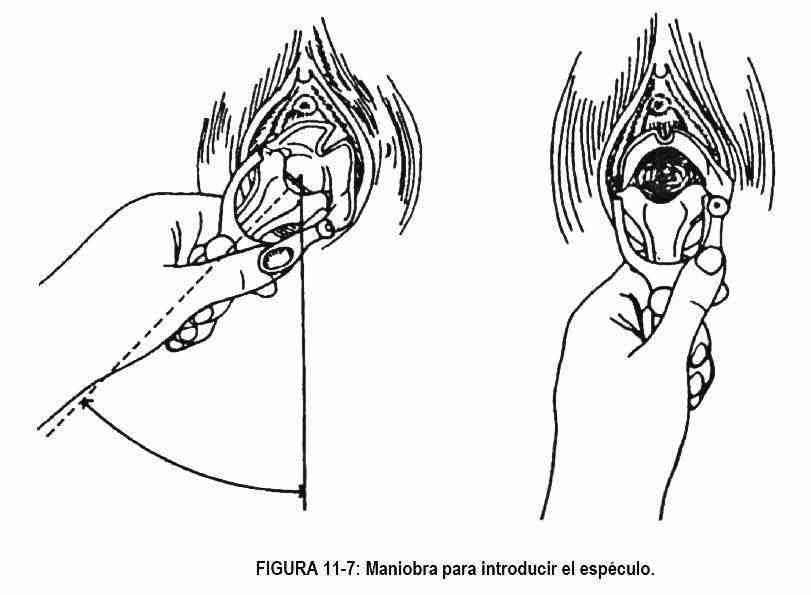
 The speculum must be placed slowly and firmly; Two exploring fingers are placed on the perineum, separating the lips to visualize the introitus, and the speculum is introduced obliquely, at 45 ° (Figure 11-7), resting on the posterior wall of the bladder (Figure 11-6, B). The speculum must be inserted laterally; Once fully inserted, it is rotated and opened, leaving an upper and a lower valve, and thus exposing the cervix; in advance the patient is warned that she is going to feel pressure.
The speculum must be placed slowly and firmly; Two exploring fingers are placed on the perineum, separating the lips to visualize the introitus, and the speculum is introduced obliquely, at 45 ° (Figure 11-7), resting on the posterior wall of the bladder (Figure 11-6, B). The speculum must be inserted laterally; Once fully inserted, it is rotated and opened, leaving an upper and a lower valve, and thus exposing the cervix; in advance the patient is warned that she is going to feel pressure.
The shape, color, and position of the cervix should be evaluated. The shape of the neck will vary according to the age of the patient and the existence or not of deliveries. In the nulliparous patient the orifice of the neck is punctate; while in the multipara it has a slit or stellar shape. Its color should be pink. The position of the cervix is helpful in assessing the position of the uterus.
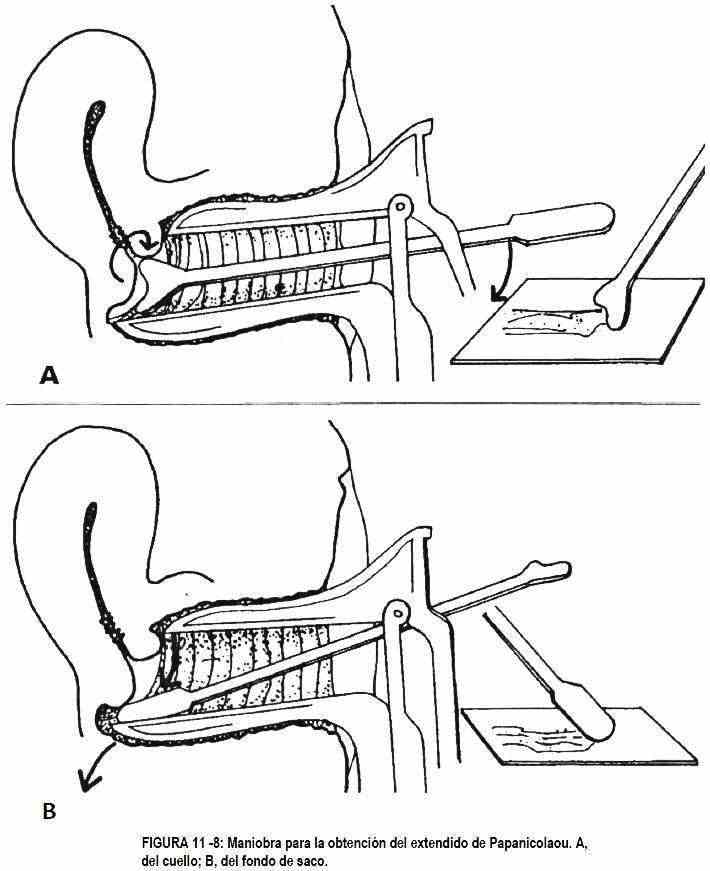
A cotton swab that is rotated in both directions should remove secretion for study (Figure 11-6, C), and with an appropriate spatula, cellular material is obtained from the cervix and vaginal wall for cytological examination (Figure 11 -6, D). A Papanicolaou smear (Figure 11-8) is performed to determine if there are cellular changes at the endo- or ectocervical canal; it can even reveal vaginal infections.
Sterile cotton and Thayer Martin culture medium are used to investigate the presence of gonococci. As soon as the speculum has been inserted and opened, the cotton is inserted into the cervical canal, allowing it to absorb the vaginal discharge for fifteen to thirty seconds.
Then it is applied to the culture medium with a rolling motion, closing the tube or container containing the medium.
The wet saline preparation is commonly used for the identification of motile trichomonads and to observe the characteristic cells of Haemophilus. It can also be moistened with potassium hydroxide to identify fungi. It is also possible to identify other germs with the Gram-Nicolle stain. This time can be used to obtain a clean urine sample.
All these studies will be carried out before applying lubricants. The patient must not have been sanitized in the last twenty-four hours. Gonococcal culture can be done during menstruation if bleeding is minimal, but Pap smear and discharge samples are not reliable unless bleeding is minimal.
By removing the speculum with the screw loose and open with the fingers, the walls of the vagina are inspected. Under normal conditions, it is possible to observe the presence of mucus in the vagina, produced by the Bartholin glands and cervical cells. This mucus will vary during the menstrual cycle, with sexual arousal, pregnancy, stress, anxiety.
The presence of mucus is controlled by the fluctuation of the reproductive hormones, mainly estrogens and progesterone. The levels of these hormones are regulated by a complex balance between the central nervous system, the hypothalamus, the pituitary, and the ovaries. The interplay between these glands and systems produces changes in the menstrual cycle, including the amount and consistency of mucus.
At the beginning of the cycle, both estrogens and progesterone are at low levels; As the cycle progresses, estrogen levels rise to trigger the production of luteinizing hormone, which causes ovulation. This increase in the level of estrogens is the cause of mucus secretion. When there are low levels of estrogen, the mucus is thick; On the other hand, when the estrogenic level increases, the mucus becomes thin, watery, translucent, elastic, acellular and with the consistency of egg white. This mucus is fertile and helps sperm motility. With ovulation, estrogen levels fall, and from this point on progesterone predominates. The mucus dries up and becomes more rubbery. Monitoring these characteristics can alert the patient to her fertile days.
The vaginal examination is carried out by introducing the index and middle fingers of the gloved and lubricated exploratory hand with sterile substance; the knob must not touch the glove. The index finger is inserted, palm down, palpating the vaginal walls and identifying the cervix. Then the middle finger is inserted and the palm is taken upwards. Later they will serve as support for bimanual palpation.
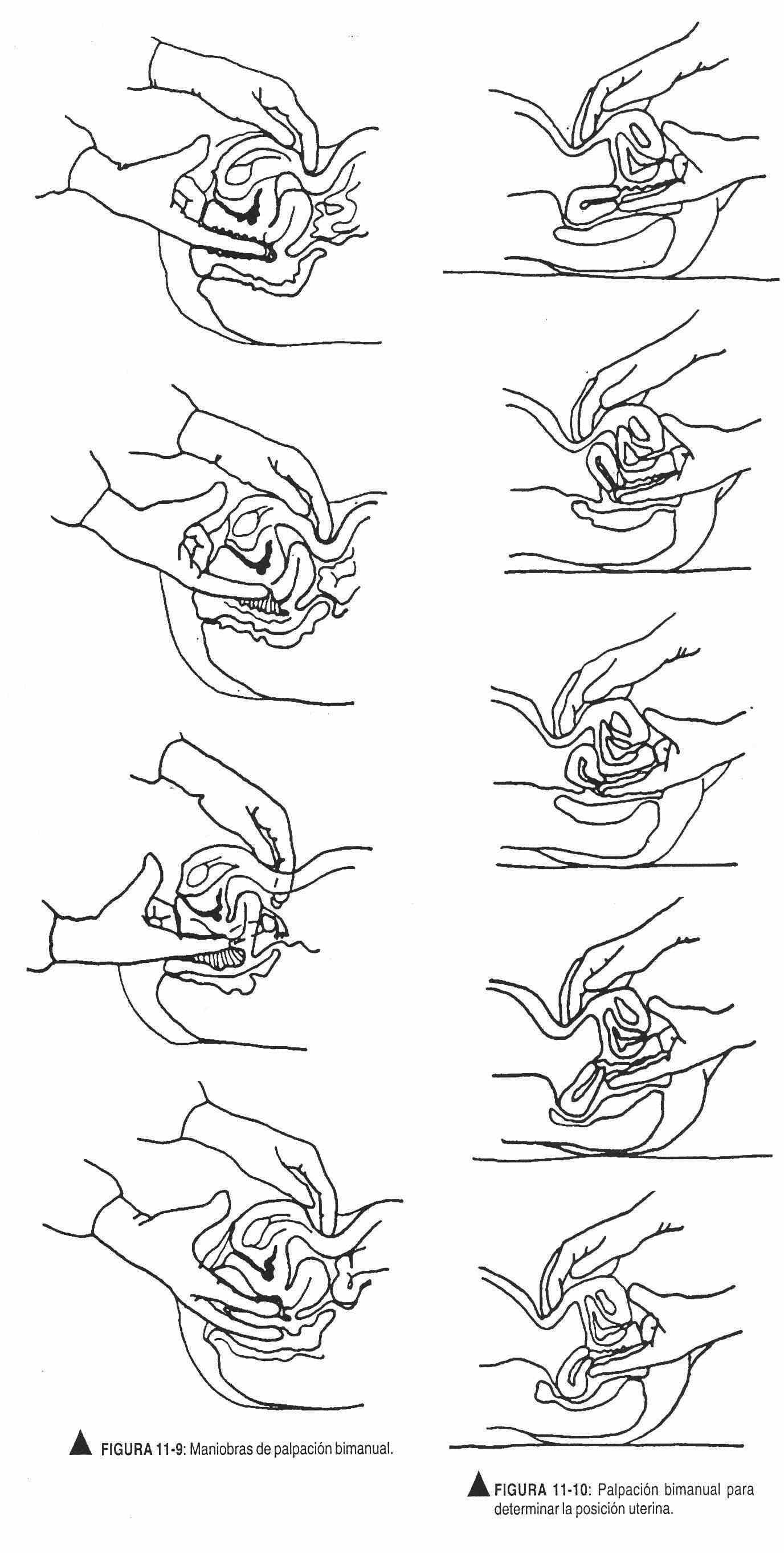
The vaginal walls and cervix should be palpated, evaluating its shape, limits, surface, consistency, sensitivity and mobility, also palpating the cul-de-sac. The abdominal hand, without a glove, between the umbilicus and the pelvis, will assist with bimanual palpation, a maneuver used to examine the ovaries and adnexa and determine the position of the uterus (Figure 11-9).
It begins by palpating the uterine fundus, describing its shape, position, sensitivity and the eventual presence of masses; deep breathing will help the patient relax. Both hands, abdominal and vaginal, work together to obtain the sensation of the uterus.
Gently removing the fingers from the cervix, they are inserted into the fornices on the side to be palpated; avoid scratching the neck with the fingers.
The abdominal maneuver will begin at the level of the iliac crest, sliding the hand towards the pubis with sustained pressure.
By having the ovary between the two hands, it will be perceived as if it escaped. The maneuver is repeated on the opposite side.
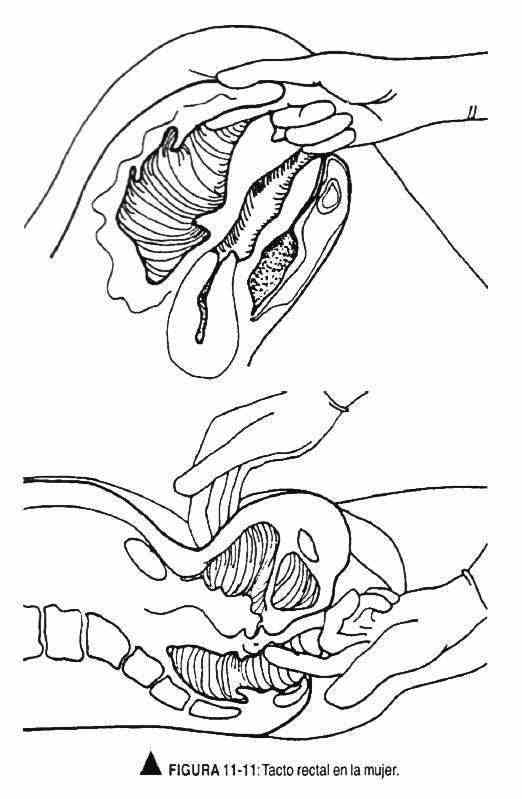
The examination of the patient can be completed by changing the glove and inserting the index finger into the vagina and the middle finger into the rectum, to assess the posterior wall of the vagina. The retroverted uterus can only be palpated in this way.
The uterine position can vary according to two factors: rotation and flexion. The version refers to the position of the body with respect to the longitudinal or axial axis of the vaginal canal, and in this sense retro means posterior to the axis, ante means anterior and middle means that it coincides with the vaginal axis; flexion, in turn, refers to the degree of rotation of the body. All of these positions are normal and have no effect on fertility (Figures 11-10 and 11-11).
At the end of the exam, the patient should be helped to sit up and offered a towel to wipe off excess lubricant, and details about the exam will not be discussed until she is dressed.