by Alberto J. Muniagurria and Eduardo Baravalle
TORAX
It includes the examination of the skin, the musculoskeletal structures, the breasts, the respiratory system and the cardiovascular system.
To examine the thorax the patient is placed in a sitting position, facing the doctor, breathing calmly and with adequate lighting.
The examination is performed by inspection, palpation, percussion, and auscultation. This examination begins with the inspection of the skin, in the anterior and dorsal aspect of the thorax, and with the palpation of the osteoarticular structures of the thorax, and with the percussion of the thoracic spine. The respiratory system is then examined by inspection, palpation, percussion, and auscultation. Then the breast exam begins in the sitting position (see Chapter 9). The patient is placed in the 45 ° supine position to complete the breast examination and to perform the cardiovascular examination (see Chapter 8).
RESPIRATORY APPARATUS
Examination of the respiratory system includes inspection, palpation, percussion, and auscultation. The chest X-ray, from the front and in profile, should be part of the complete chest examination.
Inspection
The inspection should take into account the underlying anatomical structures. For this, it is useful to know the anatomical landmarks, namely: a) the angle of Louis or angle of union of the sternal manubrium with the sternum, which coincides with the second costal cartilage and is used as a reference point to count the costal arches and intercostal spaces; b) the clavicles; c) the shoulder blades, the lower limit of which is at the level of the seventh rib; d) the prominent process of the seventh cervical vertebra; and e) the epigastric angle, with the apex formed by the xiphoid process and the sides by the last costal cartilages.
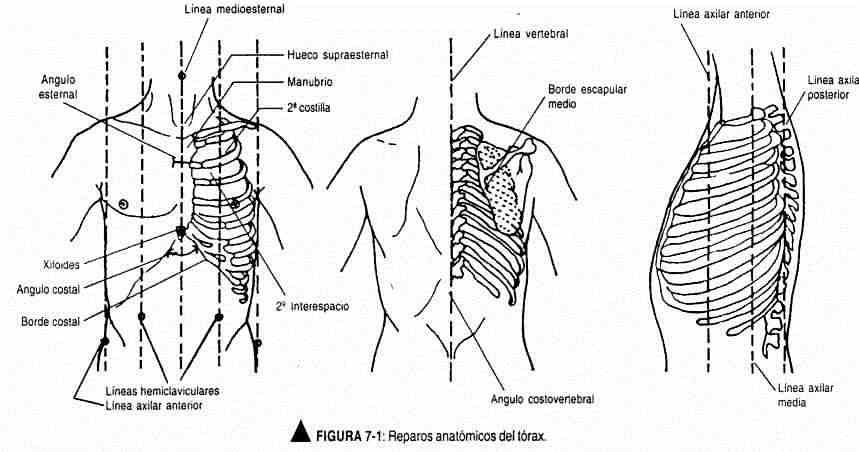
You must also know certain imaginary lines (Figure 7-1) that help to limit or locate certain areas: a) the mid-sternal line is a vertical line that passes through the middle of the sternum; b) the hemiclavicular line is also vertical and is drawn from the midpoint of the clavicle; c) the posterior axillary line is located parallel to the posterior wall of the axilla; e) between both axillary lines, at a point equidistant from one to the other, is the mid-axillary line; and f) the vertebral line coincides with the spinous processes.
It is important to know the representation of the lobes and bronchopulmonary segmentation in the chest walls. The right lung is larger and divided into three lobes: upper, middle, and lower. The left lung is smaller, due to the space that the heart occupies, and has two lobes: upper and lower. Each lobe is covered by the visceral pleura, thus forming the fissures. The right lung has a major fissure and a minor fissure. The greater fissure separates the upper from the lower lobe and, further forward, the middle from the lower. It runs from top to bottom and back to front, starting from the fifth dorsal vertebra to the costophrenic angle. The minor fissure separates the upper lobe from the middle lobe; part of the fifth rib at the level of the mid-axillary line and reaches the fourth rib in the forelimb. In the left lung, the greater fissure separates the upper lobe from the lower lobe, and runs from top to bottom and back to front. Therefore, on the right side the examination of the anterior chest wall allows the evaluation of the middle lobe and the upper lobe. On the left side, the upper lobe is examined in front and the lower lobe behind. The lower limit of the lungs lies behind at the level of the tenth costal arch, reaching the twelfth rib in inspiration. This, along with a schematic of the segmental lung anatomy, is seen in Figure 7-2. and it goes up and down and back and forth. Therefore, on the right side the examination of the anterior chest wall allows the evaluation of the middle lobe and the upper lobe. On the left side, the upper lobe is examined in front and the lower lobe behind. The lower limit of the lungs lies behind at the level of the tenth costal arch, reaching the twelfth rib in inspiration. This, along with a schematic of the segmental lung anatomy, is seen in Figure 7-2. and it goes up and down and back and forth. Therefore, on the right side the examination of the anterior chest wall allows the evaluation of the middle lobe and the upper lobe. On the left side, the upper lobe is examined in front and the lower lobe behind. The lower limit of the lungs lies behind at the level of the tenth costal arch, reaching the twelfth rib in inspiration. This, along with a schematic of the segmental lung anatomy, is seen in Figure 7-2. coming in inspiration to the twelfth rib. This, along with a schematic of the segmental lung anatomy, is seen in Figure 7-2. coming in inspiration to the twelfth rib. This, along with a schematic of the segmental lung anatomy, is seen in Figure 7-2.
The inspection should begin by evaluating the respiratory rate, rhythm, thoracic symmetry, respiratory expansion, and the auscultated inspiration / expiration ratio, which is 2: 1 under normal conditions. This same ratio, on inspection, is normally 1: 2.
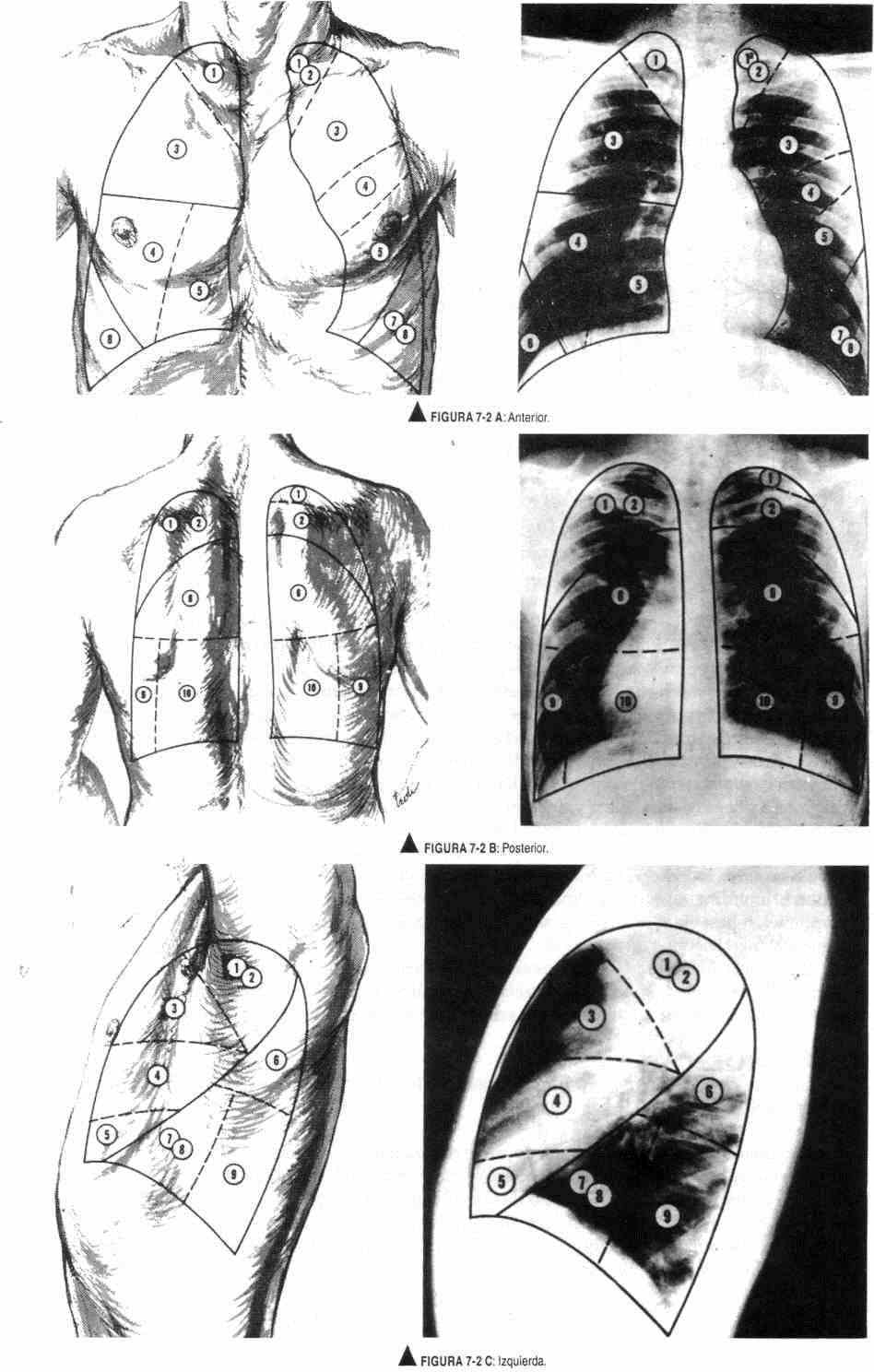
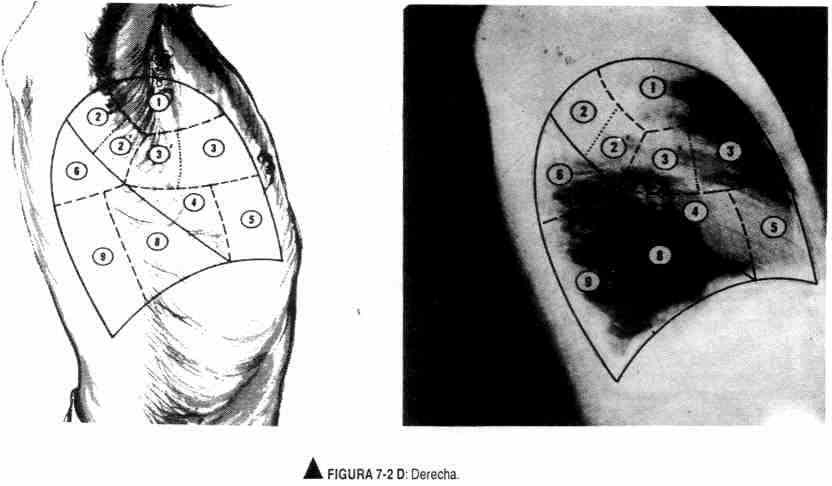
Figure 7-2. AD. Segmental lung anatomy. In the radiographs, the bronchopulmonary segments have been delineated as they are projected on the surface of the lung and, consequently, on the thoracic wall, where the physical findings can be referred separately to their respective location. The lines do not necessarily represent the radiographic projection of the entirety of each segment. All projections on the outer wall of the thorax are drawn to correspond to the position in which the radiograph is taken. The solid lines represent the interlobular fissures; the dotted ones, the segmental planes. The segmental bronchopulmonary nomenclature depends on the anatomy and the nomenclature of the corresponding bronchi. (Taken from Judge and Zuidema: The clinical examination. El Ateneo, Buenos Aires, 19).
| Right lung | Left lung |
|
Upper lobe Middle lobe Lower lobe |
Upper lobe Upper Lower lingual division Lower lobe |
* These axillary subdivisions are included as such due to the frequency with which they are affected together, independently of the rest of their respective segments.
** The middle basal segment is not represented on the surface of the lung below the chest wall.
*** The apical-posterior and basal anterior-middle segments of the left lung are considered segments with subsegmental subdivision, because each of them receives a single segmental bronchus. In some classifications the posterior segment is mentioned as 3, the anterior segment as 2.
Palpation
Palpation of the respiratory system includes palpation of respiratory expansion and vocal thrill.
Respiratory expansion. This maneuver is performed to check the volume changes that occur in the lungs with inspiration and expiration. With the thumbs at the level of the tenth dorsal vertebra and with the rest of the hand resting flat on the rib cage, the opening of the angle thus formed can be observed, which occurs with respiratory movements and the symmetry of this movement (Figure 7- 3). This maneuver can also be performed from the front with the thumbs at the epigastric angle
Vocal thrill . The vibrations produced by the articulation of the word are transmitted to the thoracic wall by the bronchopulmonary tissue. They are perceived at the level of the chest wall as a palpable vibration or thrill. Their presence should be evaluated and compared in both lung fields; they are usually most intense in the anterior chest wall, where the bronchi are relatively further away from the wall. They increase with the severity of the voice and with the greater intensity of it. They are also used to assess the lower lung limits.
This maneuver is performed with the palmar surface of the fingers resting gently on the posterior wall of the thorax, following an imaginary interscapulovertebral line that moves away from the vertebral column below the scapulae.
Each time the fingers rest on this line the patient should say "thirty-three". Once both lines have been probed, the comparative probing will be carried out. The same maneuver is performed on the anterior chest wall, following the hemiclavicular lines. Under normal conditions, the vocal thrill will be absent or decreased in the cardiac area. The vocal vibrations will be strongest near the source bronchi and weakest in the peripheral areas.
To evaluate the lower pulmonary limits, the ulnar border of the hand is used until the point where the vocal vibrations disappear (Figure 7-4) is found.
Percussion
Percussion of the chest produces audible sounds and palpable vibrations that allow the parenchyma to be distinguished with air, liquid, or solid. It is used to check the existence of normal lung loudness and compare it with that of the opposite side, and to determine the level of the lung bases and the excursion of these.
This maneuver is performed from top to bottom, following the interscapulovertebral line, intercostal space by space, placing the pleximeter finger parallel to the costal arch, until it surpasses the shoulder blades, where it gradually moves away from the spine. Both lung fields are percussed, and then comparative percussion is performed. A sonorous sound should be obtained.
Upon reaching the lower limit of the lungs, the change from normal loudness to the dull sound of the diaphragm will be observed.
To evaluate the excursion of the bases, the patient is asked to take a deep inspiration with percussion to the lower limit of loudness. A normal loudness will be observed during inspiration and dullness during expiration. Loudness or lung excursion usually reaches the level of the twelfth dorsal vertebra.
In the anterior wall it is struck following the hemiclavicular line. In the hemithorax following the hemiclavicular line. In the left hemithorax the cardiac submatidity will be found, while on the right side the pulmonary loudness should be found, then the submatidity produced by the lung and liver, and further down the liver dullness.
Auscultation
Respiratory auscultation can be direct or indirect. Direct auscultation is performed by applying the examiner's ear to the thoracic wall, with the help of a cloth, avoiding being made of nylon so that no added noise is produced. Indirect auscultation is carried out with the stethoscope.
The patient should be in a sitting position, with the arms crossed forward to separate the shoulder blades and then raise the arms to be able to listen to the armpits; later, the anterior chest wall will be auscultated. If there are voluminous breasts, the patient will be asked to lift them. Nylon clothing should not be listened to because of the added noise it generates. Other causes of added noise are hair and shaking.
The stethoscope must be firmly applied to the chest wall. If the hood is used, it can be applied with more pressure so that the patient's skin becomes a membrane. The examiner must be careful not to breathe on the stethoscope tubing to avoid generating added noise. The patient will be instructed to breathe with the mouth open, more deeply and more frequently. As the auscultatory act is performed, you will be told if it is necessary to do it more deeply, or more or less quickly than cough, to say letters like "i" and also words like "thirty-three".
The stethoscope should follow an auscultation line in both hemithorax, first on one side, then the other, and then comparatively, covering all bronchopulmonary segments.
If a beginner leaving a concert is asked to describe the sonic characteristics of the piano, it is likely that he has not paid attention to it. When you listen to the concert again, your attention will be directed exclusively to the sound of the piano trying to cancel out the rest of the instruments. This concentrated effort to separate auscultatory phenomena requires a methodology that must be learned. In pulmonary auscultation, therefore, the following steps will be followed:
- Detect respiratory sound
- Assess inspiration
- Assess expiration
- Assess the inspiration / expiration ratio
- Investigate the presence of added noise
- Make the patient cough
- Auscultate the voice
Acoustics . Pulmonary sounds are produced by rapid fluctuations in gas pressure or by oscillations in solid tissues; they can be dimmed or filtered when transmitted to the stethoscope.
Flow patterns . The gas that runs through a tube flows in a laminar fashion. There are no sudden changes in pressure oscillations capable of generating sound waves. The gas flow in the terminal bronchi and alveoli is silent.
However, above a critical flow velocity the streamlines break, and small patches of gas begin to move crosswise and against the flow direction (turbulent flow) producing fluctuations in gas pressure, and thus causing noises that vary between 200 and 2000 Hertz. By analogy with the spectrum of white light, they are called white noise.
The critical speed point depends on inertia and viscous forces, which is expressed by the Reynolds number, calculated according to the following formula: Reynolds number = (Flow velocity x gas tube diameter) / Vicosity of the gas
In the bronchial tree, it also depends on obstacles to flow and abrupt changes in flow direction. In the trachea and the large bronchi the flow is turbulent, and laminar in the peripheral bronchi where the Reynolds number is less than one. Between both areas (segmental bronchi-fifth generation bronchi) the flow is cut by vortices.
Vortices . When a gas stream passes from a circular groove or hole into a larger or directional passageway, forces are created at the boundary of the gas jet and the surrounding fluid. These forces have a circular sense and move at different speeds. They are called vortices and they originate when the Reynolds number reaches a critical value. Above this number, the appearance of vortices depends only on the speed of the gas.
Technical aspects . The stethoscope will be efficient if it transmits high and low frequency sounds well. Lung sounds have a wide range of frequencies. The added noises are low; instead, breath sounds are close to the threshold of hearing and may go unnoticed in a noisy environment if the stethoscope is not appropriate.
Measurements . It is possible to measure the intensity of sound waves to assess intensity and frequency. Basically, the device consists of a microphone, a recorder and an oscilloscope, connected to the mouth. Measurements on the wall are more difficult, since these sounds are weak and prone to being modified by depression on the microphone and the skin. There are UV light recorders that may be more useful in research.
Intensity . Due to the great variation in amplitudes between weak and strong sounds, they are compared on a logarithmic scale. The unit is the decibel. Within certain limits the correlation between airflow and the amplitude of sounds is linear.
Transmission . The transmission of sound through the thorax is measured by comparing the intensity of the sound of the voice in the mouth and in the chest wall, which are recorded simultaneously, and with a stereo recorder they are integrated into an operational amplifier in analog or digital way, comparing the loss of energy between the two.
Bronchial sound or noise. Vesicular murmur (respiratory sound) . These sounds or noises are produced by respiratory movements. They have a variable amplitude that oscillates between 200 and 2000 Hz.
There are important differences between the sounds heard in the mouth and those heard in the chest wall. Normal breathing is barely audible in the open mouth and is heard as a whisper, which is known as a white sound. It is a turbulent flow and is composed of a great variety of frequencies.
The bronchial sound and the vesicular murmur originate in the turbulent flow of the respiratory tree, from the mouth to the segmental bronchi, with the possible contribution of vortices from some more peripheral zone. Sound travels well in gas with a turbulent flow of the airway from the trachea to the segmental bronchi. The small bronchi offer resistance to gas oscillations in acoustic frequencies. Therefore, beyond the segmental bronchi, respiratory sound travels through the lung parenchyma. The intensity of the auscultatory phenomenon heard on the wall will depend on the distance between the sound source and the wall. In its transmission to the wall, the sound is attenuated and filtered by the lung tissue. At the level of the mouth, frequencies of 200-2000 Hz are heard;
Bronchial sound or laryngotracheal noise is a high pitched, inspiratory and expiratory sound. Onomatopoeically as the letter G. It is heard in the trachea and the source bronchi.
The vesicular murmur or respiratory sound is a low-pitched, soft and musical sound, which is heard on inspiration. On expiration it occupies the first third of the expiratory moment. It is heard at the level of the thoracic wall, especially the posterior wall. The onomatopoeia is the letter V.
The source of the bronchial sound and the vesicular murmur is at the level of the large bronchi and not at the level of the respiratory bronchioles and alveoli, as was thought in the 19th century.
It is correlated with air flow, that is, with pulmonary ventilation. As is understood, there may be regional differences. At the bases it is more intense at the end of inspiration, and at the apex it will become weaker as inspiration passes.
Auscultation of the voice . The voice has mainly low-frequency sounds, 150 Hz in men and 230 Hz in women. Each vowel has a pair of partial frequencies that can reach 400-2400 Hz. These partial tones, called formants, have a frequency independent of the fundamental tone that is the same for men and women. When the formants are lost in transmission, speech becomes incomprehensible.
Low sounds, up to 200 Hz, are well transmitted. As a result, most of the vocal formants are lost and speech is heard on the wall as a murmur or unintelligible sound. The voice heard at the level of the trachea is understandable.