by Juan C. Linares Casas, Alberto J. Muniagurria and Eduardo Baravalle
The examination of the cardiovascular system includes the examination of the jugular venous pulse, the arterial pulse, the blood pressure and the cardiac examination carried out through the anterior wall of the thorax. To fully understand the cardiovascular system, it must be taken into account that this system is made up of chambers and pipes, which hold different pressures. These pressure differences generate a movement of liquids in the pipes and in the chambers.
In different regions of the body, movements and noises can be detected that help the doctor to locate himself at different times of the cardiac cycle.
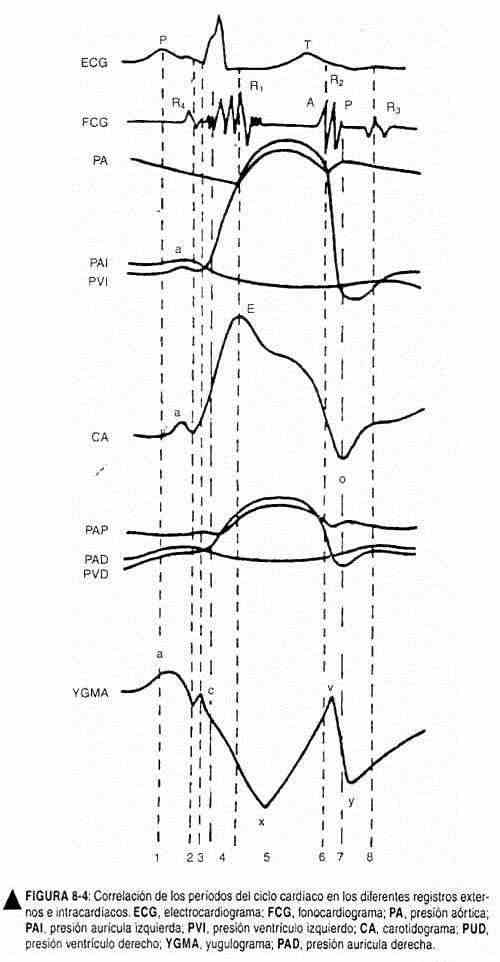
It is convenient for the student of this methodology to know in detail the physiology of the cardiovascular system, both in its mechanical and electrical parts, in order to interpret the findings of the physical examination. That is why it will be extremely useful to know the different graphic records of the venous pulse, the arterial pulse, the left ventricular impulse, the electrocardiogram and the phonocardiogram in isolation and in combination. Together, the arterial pulse, the left ventricular impulse (IVI), and the heart sounds record the activities of the left chambers. Venous pulse is the hemodynamic parameter of the right chambers. The findings of the examination of the cardiovascular system have a high correlation index with the findings made at the necropsy of the patient.
VENOUS PULSE
The venous pulse, cervical venous pulse or jugular venous pulse, is a volume wave seen on inspection of the internal and external jugular vein on the right side of the neck. It is a clinical element of great value, which expresses the dynamics of venous return to the right heart. The venous pulse waves reflect the changes in volume of the right atrium at each moment of the cardiac cycle. Venous pressure indicates right atrial pressure. These data allow to obtain valuable information on the filling of the right ventricle.
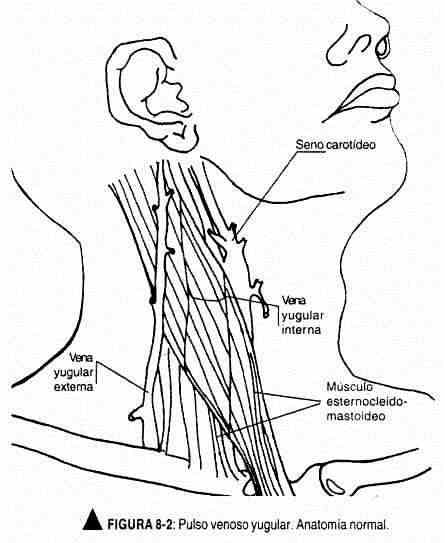
Exam technique. The pulsatile wave should be sought in the area of clavicular insertion of the sternocleidomastoid muscle, which is where the internal jugular vein is located, or directly in the external jugular vein. The latter can go unnoticed in cases of venous hypertension. Therefore, to measure venous pressure, the oscillating end of the venous pulse of the right internal jugular should always be taken as a reference (Figure 8-2).
The patient should be in supine position with the head of the bed elevated at 45 °. In this position, the oscillating end of the jugular vein is immediately above the clavicle. As the patient reclines, the level will rise along the neck until it is hidden at the mandibular angle. In the upright position, however, the pulse will disappear behind the clavicle.
Although the ideal is to work with a bed with a moving head, this is not always possible. If a pillow is used to bend the patient, it should include the shoulders; otherwise, flexing the neck may make observation difficult.
The doctor should be located to the right of the patient and have a tangential light that favors the production of faint shadows, which will facilitate the vision of the pulsating wave. The patient should turn the face to the left, while the doctor, with his right hand, should search for a nearby arterial beat to use as a reference in the cardiac cycle. This beat can be the left carotid beat or the left ventricular impulse.
The venous pulse should be evaluated on the right side of the neck, since in 25% of normal people a jugular engorgement can be observed on the left side due to the presence of the innominate artery that compresses the jugular vein.
Venous pulse characteristics. There are elements that clearly define the venous pulse, which were studied by T. Lewis and P. Wood: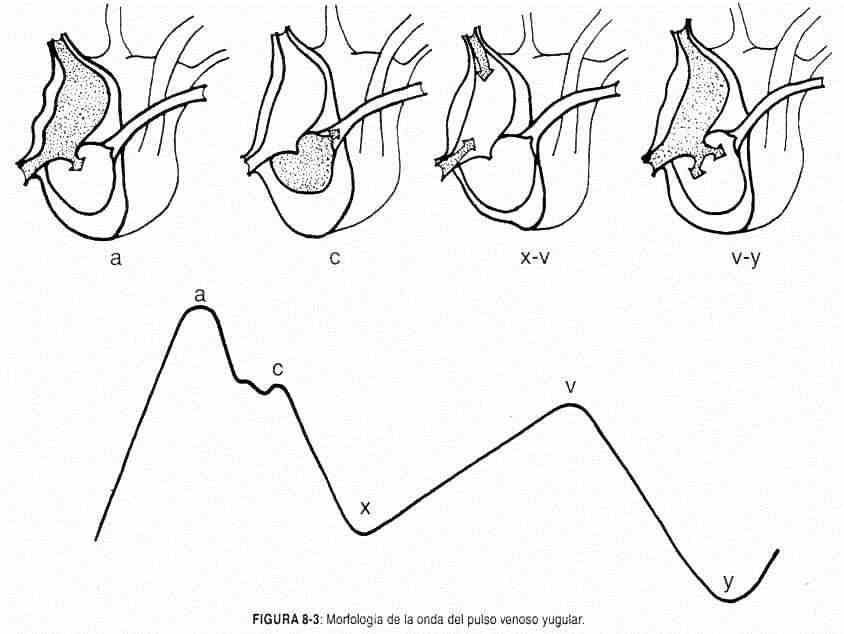
- the venous pulse is smooth, diffuse and undulating, like the tide;
- since it is a volume wave, it can be seen, but not felt;
- the level of the wave varies with respiration, passively following changes in intrathoracic pressure. It descends in inspiration and rises in exhalation:
- the pulse level varies with changes in posture following the influence of gravity, and is therefore higher in the horizontal position than in the vertical;
- if the jugular veins are compressed at the base of the neck, the venous pulse will disappear and the jugular veins will become engorged;
- abdominal compression normally raises jugular venous pressure, sometimes by increasing venous filling pressure and other times by modifying intrathoracic pressure; this is momentary.
- the most striking feature of the venous pulse is its configuration.
Venous pulse configuration. For each cardiac cycle, the venous pulse consists of two waves with four crests (a, c, v, and h) and two sinuses (x and y) (Figure 8-3).
The crest a (or wave a) (atrial) is due to atrial contraction; it is thus presystolic, and precedes the carotid beat. The sinus x is the dominant wavelength of the venous pulse; it is almost certainly produced by the relaxation of the atrium (atrial diastole), thus expressing the decrease in atrial pressure during the expulsive phase of ventricular systole, and is responsible for the classic systolic collapse of the venous pulse. It should be noted that some authors consider that sinus x is caused by the systolic displacement of the tricuspid plane towards the tip. The c (carotid) ridge , often interrupting the x sinusdescending, was attributed by Mackenzie to the contiguous effect of the carotid pulse. It occurs during the ejection phase of ventricular systole.
The v (ventricular) crest corresponds to the filling of the right atrium and is believed to be due to an increase in intra-atrial pressure due to the bulging of the tricuspid valve. It begins at the end of the expulsion phase. Its upward stroke is due to the progressive accumulation of blood in the atrium and vena cavae, while the tricuspid valve remains closed. Its vertex corresponds to the opening of the latter, that is, to the venous emptying.
The descending sine y is the descending slope of wave v , as is the sinus x of wave a , and therefore expresses the phase of rapid ventricular filling. It is, therefore, a diastolic sinus (x is systolic), little marked, because in normal conditions the blood pressure difference or right atrioventricular gradient is small and the pressures equalize quickly.
The h ridge is small and of little clinical value. It occurs if the heart rate is low. In normal conditions it is not visible, but can be registered at the end of the sinus and .
Therefore, and unlike the arterial beat, the venous pulse is characterized by the classic systolic collapse, because the normal dominant wave is the sinus x . To locate it in time, the first noise can be taken as a reference or, better still, the carotid pulse, which exactly coincides with the descending sinus x (Figure 8-4). The crest a , for its part, is presystolic; the v peak occurs in the latter part of systole, and breast and is clearly diastolic. All these waves are clearly distinguishable in cases of slow ventricular rate. The differences between venous pulse and carotid pulse are shown in Table 8-1.
| Table 8-1. Differences between venous pulse and carotid pulse | |
| Venous pulse | Carotid press |
| It is seen and not palpable | It is seen and felt |
| Wave a is before the first noise | Pulsating wave after the first noise |
| Diffuse and undulating | Vigorous |
| Four positive and two negative waves | A positive wave |
| Changes level with position | Does not change level with position |
| Disappears under pressure | Doesn't go away under pressure |
| Descend in inspiration | Does not descend into inspiration |
| Hepatojugular (pathological) reflux | No hepatojugular reflux |
Venous pressure.It is the other chapter of the jugular pulse examination. The height of the venous pulse is correlated with the central venous pressure. The vertical distance between the oscillating top of the internal jugular vein and the sternal angle of Louis measures the central venous pressure (CVP) in centimeters of blood, similar to centimeters of water, because the density of blood is 1.056. Lewis chose the sternal angle because it is in a fixed relationship with the right atrium, about 5 cm above its geometric center, both in the upright position and in the decubitus position. Normal jugular venous pressure ranges between +3 and -7 cm with reference to the Louis angle and with the patient in a horizontal position (Zarco) (Figure 8-5). When estimating central venous pressure it is necessary to indicate the position of the patient,
CARDIAC EXAM
Inspection and palpation of the precordium
Inspection and palpation of the precordium have been thoroughly studied and perfected in recent years; they provide data of remarkable utility and accuracy. These maneuvers presuppose knowing the location of the cardiac and vascular structures that are behind the chest wall. The right ventricle is located in the fourth and fifth left intercostal spaces, while its infundibulum and pulmonary artery project into the third and second left intercostal spaces, adjacent to the sternum. The right atrium, on its right border, is located in the lower portion of the right sternal border, while the left atrium is behind the right ventricle and only the appendage protrudes at the level of the left third intercostal space. The aortic root projects to the right of the sternum,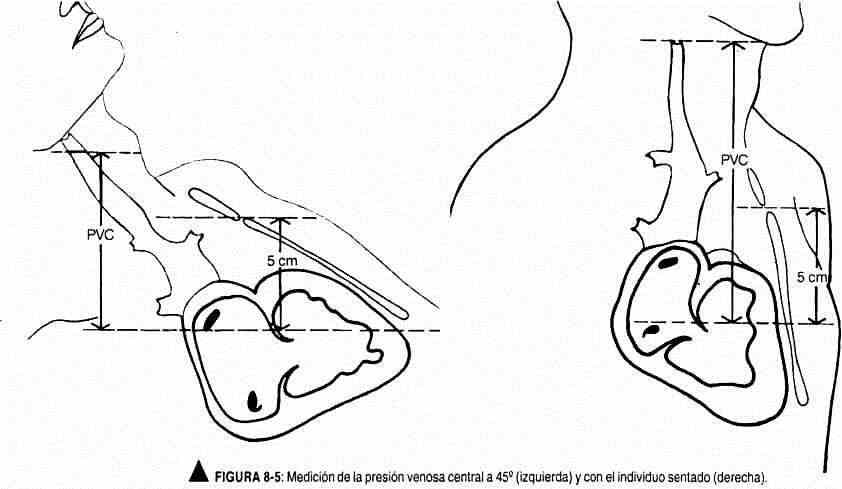
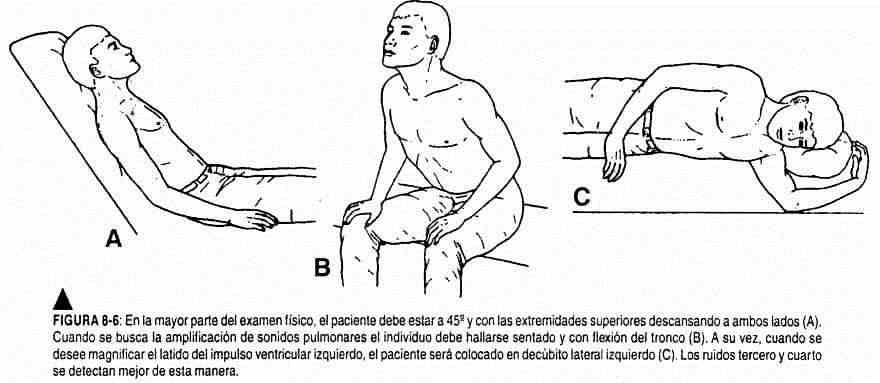
The clinical examination should be performed with the patient in the supine position with the head slightly raised or, better still, with the trunk tilted 30 ° or 45 ° from the horizontal, and then in the left lateral decubitus (Figure 8-6). The use of a flashlight is recommended to project a tangential light on the various thoracic and cervical regions. This will make the elevations and retractions of the different areas under examination more evident. The physician should stand to the right of the patient. He will palpate by placing his right hand on the precordium, first covering the apexal region, then the mesocardium and the lower sternal region, and finally the base on both sides of the sternum, taking the doctor's hand the shape of the heart (Figure 8- 7).
The precordial beats are generally more noticeable on inspection and palpation in children and adolescents, as well as in people with a thin chest.
Areas. For inspection and palpation, the following areas should be evaluated: a) apical or impingement of the heart tip; b) right ventricular or tricuspid area; c) pulmonary or left parasternal, at the level of the second intercostal space; d) right aortic or parasternal, at the level of the second intercostal space; e) epigastric; f) right and left sternoclavicular. To these regions must be added the area to the right of the apexal beat, up to the sternum and xiphoid appendix.
Apical area. In the apical area, the left ventricular impulse is palpated, which is usually the most notable precordial movement. It is also known by the name of tip shock, apex beat, or point of maximum intensity. It should not be confused as the precordial point of maximum intensity (PMI), since, although in healthy subjects and in many patients the two coincide, in some patients with heart disease they may be different. In many patients with right ventricular or biventricular enlargement, the PMI actually corresponds to the beat of the right ventricle.
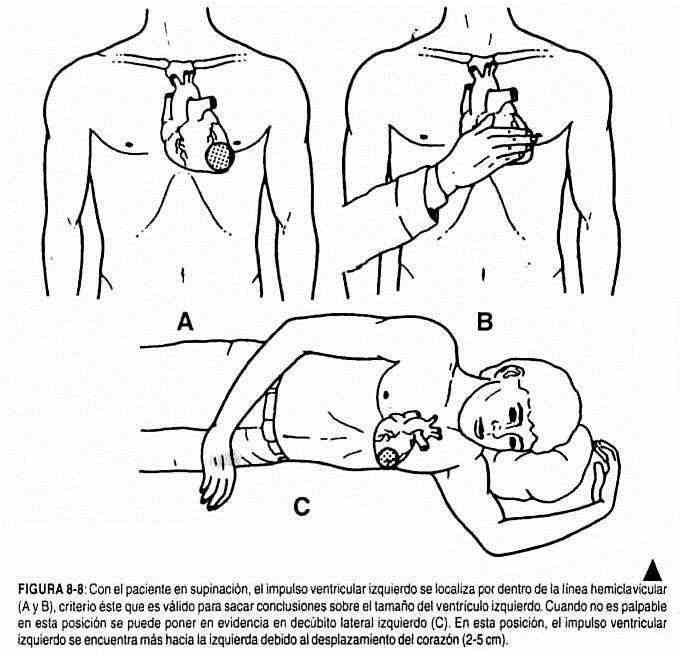
 The left ventricular impulse is palpable and is sometimes observed in normal persons at the level of the left fifth intercostal space, and exceptionally in the left third, fourth, or sixth intercostal spaces, above or within the midclavicular line. It constitutes a systolic elevation of 1 to 2 cm in diameter and 0.5 to 1 mm in width.
The left ventricular impulse is palpable and is sometimes observed in normal persons at the level of the left fifth intercostal space, and exceptionally in the left third, fourth, or sixth intercostal spaces, above or within the midclavicular line. It constitutes a systolic elevation of 1 to 2 cm in diameter and 0.5 to 1 mm in width.
It is interesting to note that the relationships between left ventricular impulse and the heart seen fluoroscopically are not always straightforward. Although the beat usually corresponds to the apex or tip of the left ventricle, it sometimes better coincides with an area 1 cm above and outside the lower left part of the cardiac silhouette (Fishleder).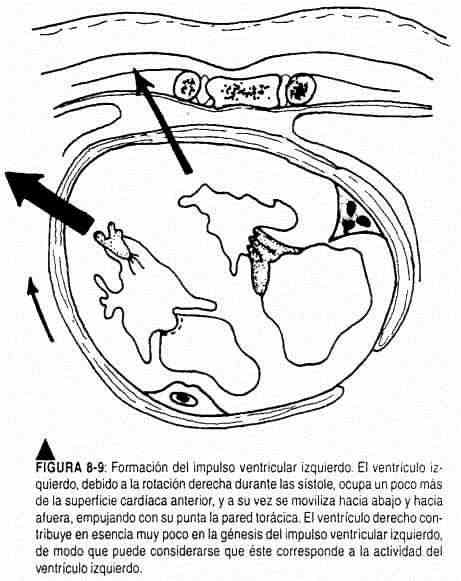
Normally the left ventricular impulse shifts 2–5 cm to the left if the individual is positioned in the left lateral decubitus (Figure 8-8) and 0.5–3 cm to the right in the right lateral decubitus position.
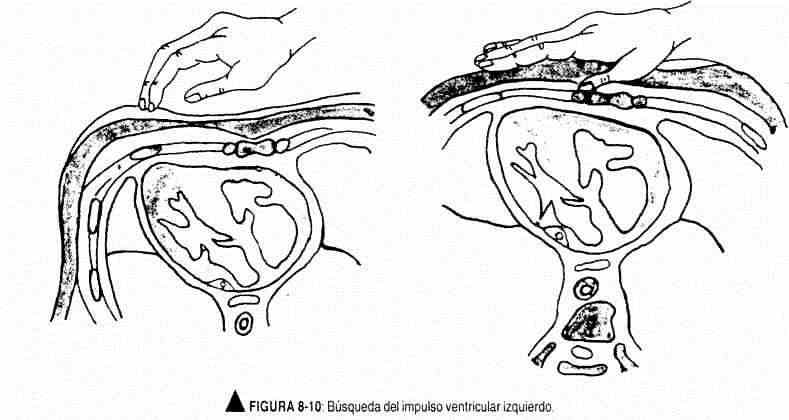
Although several factors are involved in the production of the precordial beats, the left ventricular impulse has its genesis in the twisting of the heart to the right (Figure 8-9) that results in better contact of the left ventricle and the interventricular septum with the thoracic wall, especially at the level of the left apex, with the consequent systolic rise. To examine the left ventricular impulse, the hand should be placed, palm down, on the thoracic wall, placing the ball of the fingers in the apical area described, until the geometric point of maximum impulse is located (Figure 8-10). If it is not perceived there, the patient should be placed in the left lateral decubitus and look for the beat in deep exhalation, remembering the movements that occur in the impulse when adopting the lateral decubitus. Not only should its location be specified, but also its extension and character (amplitude, duration and strength). Left ventricular impulse duration occupies the first third of cardiac systole (Figure 8-11).
Right ventricular area. This area is in the third, fourth, and fifth intercostal spaces to the left of the sternum. In normal individuals, soft pulsations can be perceived, which occasionally may be more extensive, especially in thin adults or anxious children.
Aortic area. The heartbeat in this area is always abnormal.
Epigastric or subxiphoid area. It is located at the angle formed by the xiphoid appendix and the costal cartilages. In normal, lean individuals, the aortic beat can be palpated. Palpation of this area is useful in children, trying to perceive the lower wall of the right ventricle; To do this, the hand is placed flat and upwards, with the ball of the right index finger directed towards the child's left shoulder until it impacts with the right ventricle. This maneuver becomes more evident in sustained inspiration.
Sternoclavicular area. This area includes the sternal manubrium and the right and left sternoclavicular joints. No pulsation is normally palpable.
Auscultation
Fishleder defines auscultation as the art of exploring the functions of the heart through the ear. And it is that, at present, this exploratory method has resurfaced renewed from the low levels in which it had been placed. This transformation responded to two causes: the deeper knowledge of cardiovascular physiology and pathophysiology and the confrontation of the signology not only with the autopsy findings, but also with the hemodynamics and the anatomy in the life of the patient. It could be said that auscultation is the peak stage of the clinical examination of the heart.
Brief notions of acoustics. The sounds that originate in the cardiac structures have a frequency that varies between 5 and 700 b / sec and rarely reach, for certain murmurs, values of up to 1000 b / sec or more. Remembering that sounds whose vibrations are less than 16 c / sec are not audible by man, a certain number of heart sounds fall in the infrasound zone and cannot be perceived. These are mainly caused by the left ventricular impulse and by the phenomena that occur in the course of contraction of the atria and rapid ventricular filling.
Low-frequency sounds (16-128 c / sec) are not easy to hear, as they are near the lower limits of audibility. The third and fourth noises belong to this category. Sounds of medium frequencies (128-256 c / sec) constitute the majority of auscultable sound vibrations of cardiac origin. High-frequency sounds (256-512 c / sec) are also very low intensity. Some faint diastolic murmurs of aortic regurgitation and prosthetic valve sounds belong to this group. Normal noises have almost no audible vibrations above 250 c / sec.
The stethoscope (from the Greek stetos, chest, and skopein, examine) is an instrument that makes it possible to listen to the noises originating in the body without directly applying the ear to the area under study. It was invented by Laennec in 1816. The ideal stethoscope for cardiovascular examination should have two parts, one for low frequencies and the other for high frequencies. For this reason, the binaural with a bell and membrane in a single piece is the one that has been universally extended.
The bell stethoscope is superior at auscultating faint mid- and low-frequency sounds, such as third and fourth sounds and diastolic mitral filling murmurs. On the other hand, the sensitivity of the bell will depend on the pressure with which it is applied to the wall: a gentle pressure transmits low frequencies better (third and fourth sounds, mid-diastolic murmurs); while strong pressure makes the bell behave like a membrane, turning the skin into a rigid diaphragm, and eliminates low-frequency sounds.
The membrane stethoscope filters out low-frequency noises for better perception of higher-pitched and low-intensity noises. For this reason, the membrane is much more useful in the auscultation of the base areas, especially in diastolic murmurs of regurgitation and in the splitting of noises.
There are even faint, high-frequency murmurs (in aortic insufficiency, for example) that are best heard with the bare ear and that are not perceived with the membrane stethoscope. This is perfectly in keeping with the extreme sensitivity of the human ear to high frequencies.
Auscultation technique. Auscultation is a technique that is only acquired by learning at the bedside. As Paul Wood rightly pointed out, when a skilled physician hears a faint diastolic murmur, it does not mean that he has a better hearing or a better stethoscope, but rather that he has acquired a more selective power of concentration.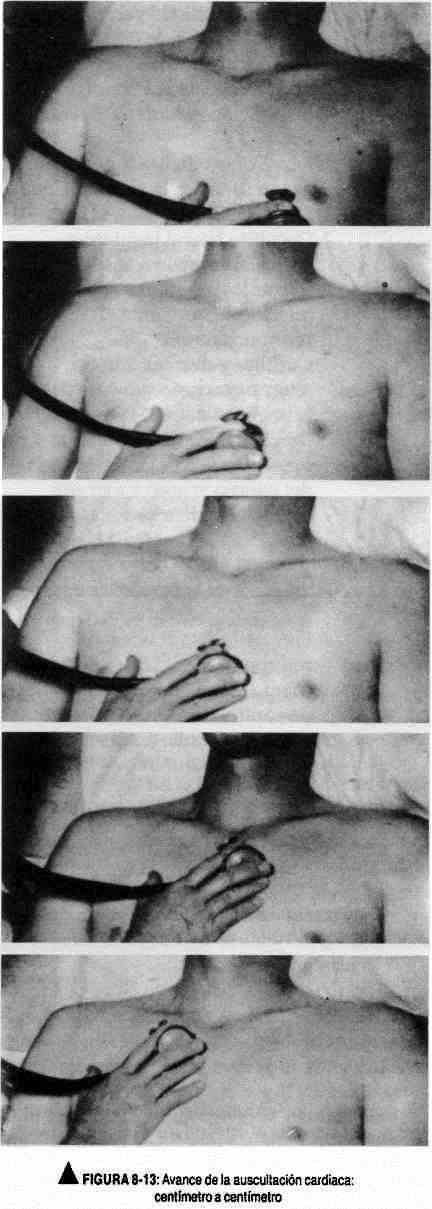
Actually, this semiological technique is fundamentally based on the explorer's ability to concentrate.
The room where it is examined should be yes] and as isolated as possible with well-lit curtains and carpets and with a comfortable temperature.
The doctor will be seated to the right of the patient, in a comfortable position. The patient, lying on a stretcher, should be comfortable and calm.
If it is a man, it will have a naked torso, and if it is a woman, a cloth should be placed during the auscultation, moving it according to the area to be examined.
Auscultation should be carried out following a systematized technique. Thus, it is necessary to know the so-called classic foci or areas of cardiac auscultation, which are the following (Figure 8-12).
- The mitral area or apical area or, better still, left ventricular area, is usually located at the level of the apex (fourth or fifth left intercostal space and hemiclavicular line).
- The tricuspid area, or right ventricular area, includes the lowest part of the sternum and the fourth and fifth intercostal spaces, 2–4 cm to the left and 2 cm to the right of the sternum.
- The aortic area is located in the second right intercostal space, next to the sternal border.
- E pulmonary l area, in the second intercostal space left parasternal. It extends up to the clavicle and down to the third intercostal space.
Although these areas and their locations are of great importance from the didactic point of view and because of their dissemination in the cardiological nomenclature, the examiner should not limit his examination to them. It is also important to examine the mesocardium, which is the area between the four areas already mentioned; the aortic accessory area, in the third left intercostal space, adjacent to the sternum, the epigastrium; the carotid and supraclavicular regions; the left axillary and infraclavicular areas and the suprasternal hollow together with the sternoclavicular joints. Auscultation will also include the thoracic dorsum, especially the interscapulovertebral space.
Auscultation should begin from the mitral area, and from there the stethoscope will be moved towards the lower end of the left sternal border, advancing a distance similar to the size of the stethoscope membrane, centimeter by centimeter. The base areas (pulmonary and aortic) will then be investigated, following the left sternal border. Subsequently, the mesocardium and the remaining areas mentioned will be explored (Figure 8-13).
Each of these regions must be explored with the hood and the membrane. Once the maximum focus of auscultation of a sound event is located, its propagation must be studied centimeter by centimeter to establish its propagation.
After this examination in supine position, the same should be repeated in other positions: left lateral decubitus, sitting, standing, and squatting.
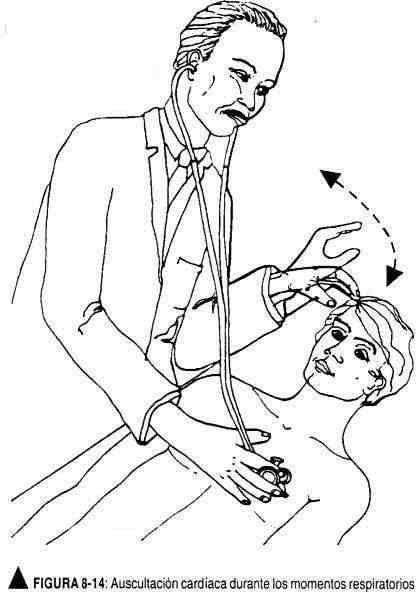
Later - or simultaneously - the changes in the phenomena auscultated during respiration will be evaluated, for which the doctor's free hand will instruct the patient to breathe in or out according to the desired change (Figure 8-14). Forced expiration with the closed glottis or Müllerian (cough) maneuvers can also be performed to exaggerate or attenuate a certain sound phenomenon.
Clinical maneuvers to modify the auscultated phenomena. The most important are the following:
- Valsalva maneuver -> decreased venous return -> decreased left ventricular volume.
- Closure of the hand -> increased peripheral resistance -> increased blood pressure -> increased pulse rate -> decreased left ventricular contratility -> decreased end-diastole volume.
- Carotid massage -> decrease in heart rate.
- Inspiration -> increased venous venous return.
Positions . There are different positions of the body that are useful in auscultation:
- Seated.
- Left lateral decubitus: brings the heart closer to the surface.
- Elevate the lower limbs -> increases venous return.
- Squatting -> decreased venous return -> increased blood pressure. If done rapidly -> increased intra-abdominal pressure -> increased venous return and in turn compression of the femoral arteries -> increased central aortic pressure, increased resistance to cardiac ejection.
- Standing -> decreased venous return -> decreased left ventricular end-diastolic volume -> increased sympathetic tone -> increased left ventricular contraction force. When standing quickly from the squatting position -> significant decrease in the diastolic volume of the left ventricle.
Pharmacological maneuvers . Inhalation of amyl nitrate -> rapidly produces a decrease in peripheral resistance with a decrease in arterial pressure and venous return and a reduction in the volume of the end of diastole in the left ventricle.
Normal auscultatory phenomena . The first thing to look for are heart sounds. Only afterwards should it be determined whether added sounds are heard.
The first heart sound is more severe, lasting and intense in the mitral and tricuspid foci. The second sound is shorter, sharp, and louder in the aortic and pulmonary foci. These noises must be correlated with the carotid pulse, which falls immediately after the first noise. The spaces between these two tones are called "silences". The silence between the first and second sounds corresponds to ventricular systole, and the silence between the second and first is longer and corresponds to diastole.
The membrane is changed to a bell to auscultate the so-called third and fourth heart sounds, which are low-toned and are heard in the lower left sternal border and in the mitral area. Subsequently, with the membrane of the stethoscope, the systole and diastole are treated in search of murmurs, clicks, clicks, etc.
First normal noise (R1) . It occurs at the beginning of ventricular systole. It is auscultated and recorded throughout the precordium, but shows its maximum intensity in the mitral focus or in the area between the apex and the left sternal border. It is lower and longer than the second tone, and contains low-frequency vibrations.
If it is desired to relate it chronologically with the carotid beat, it is observed that it begins at the end of the first sound.
Its genesis has been a controversial topic since Laennec. In 1950 forty different theories were pointed out about the causes of its production. At present, there is even no unanimity of criteria.
Rushmer proposed the theory of the "cardiohematic sound generator". According to this theory, heart sounds would be the result of accelerations and decelerations of blood flow in the chambers of the heart during the different phases of the cycle. These movements would vibrate the different cardiac structures (valves, myocardium, vessels), thus configuring the noises.
Schutz and Luisada support Rushmer's theory.
The "valve" theory, on the other hand, considers that the valves are the main generating elements of heart sounds, since they are the structures that vibrate with the highest frequency and greater intensity, especially when closing, since they are formed by thin veils and resistant. Leatham, Fishleder, and Dock hold this view.
The sequence of phenomena that make up the first noise is as follows: mitral valve closure occurs first, then the tricuspid valve, followed by the opening of the pulmonary and aortic sigmoid valves.
The mitral and tricuspid components constitute the main or audible segment of the first sound. The first of these is the most intense, and is more easily heard at the apex and the apex-xiphoid region, decreasing towards the base areas. When the Valsalva maneuver ceases (forced expiration against the closed glottis), it causes a delayed reinforcement, from the sixth to the tenth beat, of the mitral component. Tricuspid closure noise follows the previous one without interruption or is separated from it by a silent interval of one to two hundredths of a second. It is auscultated with maximum intensity at the level of the third to fifth left intercostal spaces, next to the sternal border.
Immediately after the Valsalva maneuver, the tricuspid component is reinforced, due to the sudden burst of venous blood into the right cavities. The vibrations caused by the opening movement of the sigmoid valves are subaudible. Only under pathological conditions do they increase their intensity and acquire the character of clicking sounds.
Frequently, both the mitral and tricuspid components of the first tone are identified separately together with the xiphoid appendix, thus giving rise to the physiological doubling of the first sound. This phenomenon is best heard with the patient sitting up and on expiration. It is observed in subjects
Normal young people and adults, and is due to asynchronous contraction of both ventricles due to earlier activation of the left interventricular septum.
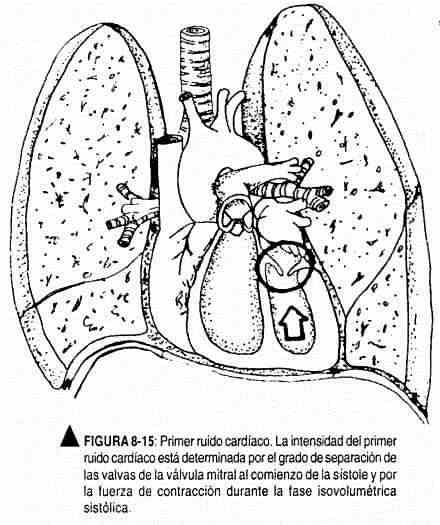
The intensity of the first heart sound depends primarily on the position of the atrioventricular valves at the onset of ventricular systole (Figure 8-15). Consequently, the first noise will be loud when these valves are wide open at systole and must go a long way to close. This occurs by prolongation of the flow path from the atria to the ventricles. In normal form it occurs when the PR space is shortened; Exercise, which is accompanied by an increase in frequency, will also increase the intensity of the first noise.
Second normal noise (R2) . The second sound is shorter and sharper than the first, and is produced by the closure of the sigmoid, aortic, and pulmonary valves, at the end of ventricular mechanical systole, when intraventricular pressure falls below systemic and pulmonary pressure. The first and second sounds therefore mark the beginning and end respectively of ventricular mechanical systole and, hemodynamically, indicate the two crucial points of intraventricular pressure change.
The second noise consists of two elements: the aortic component (A2) and the pulmonary component (P2), produced by the closure of the respective valves (Figure 8-16). The aortic component, the first, is more intense than the pulmonary in physiological conditions, it is heard as an exclusive element of the second noise in the aortic area, in the territory of the tip and in the carotids, and as a dominant element in the tricuspid area, in the third left parasternal intercostal space, and even in the pulmonary area. The weaker pulmonary component is auscultated in an area that is limited to the pulmonary focus and the left third intercostal space near the sternal border.
It is in the pulmonary area where the two components of the second sound are auscultated with a physiological doubling during inspiration. The split is mainly due to the delay of the pulmonary component during said inspiratory phase. Inspiration increases venous return to the right chambers, and thus right ventricular stroke volume, while exerting an opposite, albeit slight, effect on venous return to the left heart. Thus, during inspiration, there is a selective increase in the volume of expulsion of the right ventricle, prolongation of the right mechanical systole and consequent delay of the pulmonary component of the second tone. Simultaneously, the left ventricular systole shortens and the aortic component advances, although to a much lesser degree.
In this way, the physiological doubling of the second sound can be demonstrated in the lung area, during inspiration, in most children and young adults and even in many elderly people. It is transmitted well to the entire left parasternal area, sometimes to the aortic area, but it is never heard in the territory of the tip, unless it is formed by the right ventricle or there is pulmonary hypertension.
But it is an important fact to remember that, on expiration, due to opposite physiological conditions, the closures of the aortic and pulmonary sigmoids approach, their components merge into a single noise, or the unfolding is minimal. For this reason, expiration sets the standard in the consideration of the pathological unfolding of the second sound.
It is noteworthy that, on inspiration, not only is the pulmonary component delayed, but, as the stroke volume of the right ventricle increases, the pulmonary arterial pressure rises and the pulmonary component of the second sound is accentuated.
Third normal noise (R3) . The third noise is recorded phonocardiographically more frequently than it is heard.
It is found and recorded mainly in children and young people, at the apex or slightly inward, in a small area. It is deaf, not very intense, and is separated from the second noise that precedes it by a short silent interval ("minimal silence"). Sometimes it is more intense, especially in children or adolescents with cardiac erethism.
The conditions that favor its perception are the horizontal decubitus, the left lateral decubitus and the Azoulay position (elevation of the lower limbs of the subject in dorsal decubitus), as well as physical effort. Conversely, it turns off in the vertical position, on inspiration, and during the pressure phase of the Valsalva maneuver.
It is a mid-diastolic noise. It coincides with the sinus and the venous beat, as described by Orias and Braun Menéndez, that is, with the end of the period of rapid ventricular filling, and is attributed to sudden ventricular distention. Other authors think that its origin is valvular; it would be produced by the momentary closure of the atrioventricular valves in the first third of diastole, due to a transient inversion of the atrio-ventricular pressure gradient. But its low frequency, its similarity to the fourth sound and, above all, the fact that it is usually accompanied by a palpable shock that clearly expresses a diastolic filling wave, make it much more likely that this sound originates in the sudden ventricular distention of a "water hammer" effect.
Fourth noise or atrial noise (R4) . Normally, atrial noise is practically inaudible. Only exceptionally is it auscultated as if it were a presystolic splitting of the first sound in young subjects with a thin chest wall, with cardiac erethism. Hence, the fourth normal noise can only be studied in graphic records. The fourth audible noise, except in the rare cases mentioned, is almost always pathological.
The fourth sound coincides with the "active ventricular filling" phase and depends, not on the atrial contraction per se, responsible for the first phonocardiographic vibrations, but on the impact on the ventricle of blood flow, driven by atrial systole. It is a ventricular filling sound (Leatham) produced by a "water hammer" effect.
The fourth sound is best heard in the tricuspid area, exerting very gentle pressure with the bell stethoscope, and preferably in the left lateral decubitus position.