by Alberto J. Muniagurria and Eduardo Baravalle
The physical examination of the abdomen should be performed taking into account its topographic division and the location of the organs in the corresponding quadrants.
Inspection
 Scarring . The abdomen may present surgical and non-surgical scars, related to the patient's medical history, or they may appear on inspection without the patient having referred them during the interrogation. It is important to describe its condition, location and size. There are scars whose edges proliferate, configuring the so-called keloid scars.
Scarring . The abdomen may present surgical and non-surgical scars, related to the patient's medical history, or they may appear on inspection without the patient having referred them during the interrogation. It is important to describe its condition, location and size. There are scars whose edges proliferate, configuring the so-called keloid scars.
Scars are described by their location. The most common are: infra and supraumbilical median, right or left paramedian (which follow the external border of the anterior rectus), right subcostal, scars in the right iliac fossa and in the inguinal region. Other times, the scar is located in the hypogastrium in a transversal way, and corresponds to an aesthetic scar from cesarean section. In the lumbar region we can find lumbotomy scars.
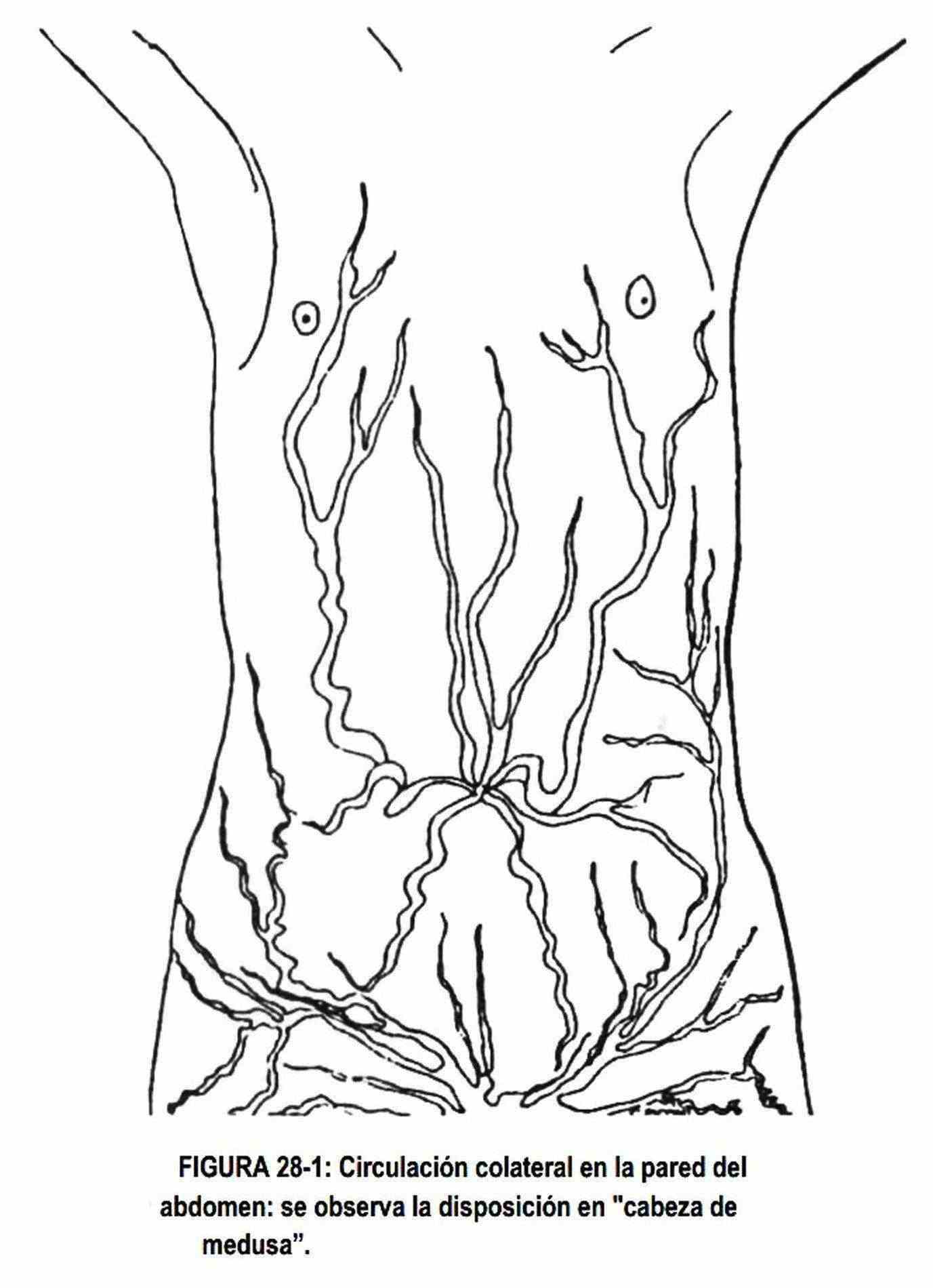
Collateral circulation. It can exist on the abdominal surface and in the upper part of the lower limbs (Figure 28-1). It is seen as dilated veins in the form of a network in the thorax and abdomen and occurs when there is an obstruction at the level of the portal circulation or the vena cava. In portal hypertension, blood is derived in part by the repermeabilized sickle ligament, and the veins dilate outward from the umbilical area, giving rise to the so-called jellyfish head. In inferior vena cava obstruction, collateral circulation develops at the level of the parietal anastomoses; in this case the blood circulates from the bottom up,
When there is obstruction of the superior vena cava, collateral circulation does not usually develop at the skin level, and blood carries through the thoracic veins to the azygous vein system.
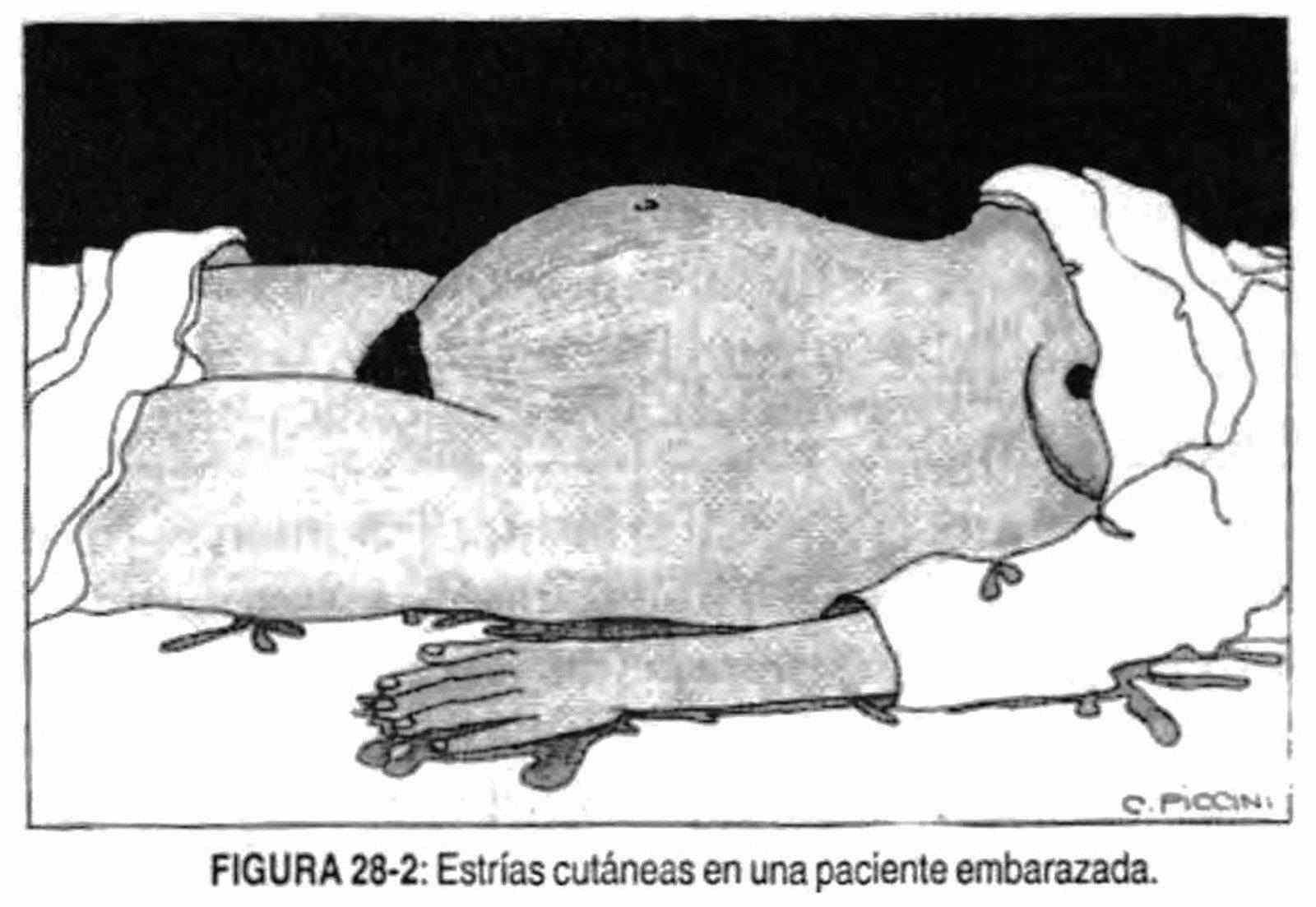
Skin . The skin of the abdomen may show stretch marks (Figure 28-2), which are commonly seen in pregnant and multiparous women. They are produced by breaking the elastic fibers of the skin. It is also possible to observe them in subjects who have undergone obvious changes in weight and in patients with large tumors. In Cushing's syndrome they are observed to be a wine-red color, while in obese and multiparous patients they are whitish.
 Form . The abdomen may be flat, protruding, rounded, or scaphoid (retracted). These features can be generalized or universal, symmetrical or asymmetric, or in localized areas.
Form . The abdomen may be flat, protruding, rounded, or scaphoid (retracted). These features can be generalized or universal, symmetrical or asymmetric, or in localized areas.
The causes of a symmetric abdominal distention are due to alterations of the abdominal wall or alterations of its contents. Among the parietal causes are obesity, wall edema or generalized or anasarca edema. Content alterations can occur at the level of an organ or the peritoneal cavity. Alterations in the cavity are generally related to the presence of fluids in the peritoneal cavity, or ascites, which when recently installed, distends the abdomen in its central part, with eversion of the umbilicus.
When the liquid spill has been in place for a long time, it overcomes the tension of the wall and distends the abdomen globally.
Characteristically everts the navel. The abdominal organs can also be the cause of symmetric bloating. Thus, for example, intestinal bloating, pregnancy, ovarian cyst and paralytic flei can cause abdominal distension. Pregnancy and ovarian cyst evert the navel.
Other times the peritoneal cavity is occupied by gas or air from the rupture of a hollow viscus or which was introduced for diagnostic purposes (laparoscopies). Localized abdominal distensions depend on causes of the wall (hernias or bruises) or content (pneumoperitoneum and visceral or tumor enlargements). A hepatomegaly, a renal cyst, a splenomegaly, a cyst of the pancreas, can produce localized enlargement of the abdomen.
Bellybutton . It may be deviated up or down, left or right, by wall retractions, or by intra-abdominal masses. It can be seen unfolded or everted in the processes that occur with abdominal distention: pregnancy, ascites, large abdominal tumors. Navel discharge can reveal umbilical infections and omphalitis; bluish discoloration of the umbilicus or periumbilical region can be seen in retroperitoneal hemorrhages and acute pancreatitis, constituting Halsted-Cullen spots. Umbilical hernias can also be seen.
Muscle development . It is closely related to the habit of the individual. Sometimes there is muscular hypotonia and a pendulous or apron abdomen is observed.
When these individuals are in the supine position, it takes the shape of a batrachian abdomen, which hangs on both sides. It is due to increases and decreases in abdominal volume, with loss of muscle tone, and sometimes to long-standing ascites. The howitzer abdomen is a prominent abdomen in the central region, in tension, and is due to pregnancy or ascites. On other occasions, there is a great muscular development that prevents the abdomen from being palpated correctly.
Universally retracted abdomens are seen in cachexia (Figure 28-5) or extreme thinning with prominence of bony landforms (pubis, iliac spines, and costal arches). It is the so-called punt abdomen. Universal retraction can also be seen in contractures accompanying an acute abdomen, meningitis, tetanus, or colic in lead poisoning.
Locally retracted abdomens are seen in cases of missing organs or shrinkage scars.
Hernias and eventrations. Hernias (protrusion of a viscus through the natural weak points of the abdominal wall) and hernias (protrusion of a viscus by defect of the abdominal muscles at the level of a surgical scar) are evident in the standing position, or when the patient raises his head or when performing positive Valsalva maneuvers. Among the hernias are described the umbilical, the direct inguinal (through the triangle of inguinal weakness), the indirect inguinal (through the inguinal tract), the crural (through the crural orifice), the white line and the lumbar. Umbilical hernias are central in children and above the umbilicus in adults, and are seen more frequently in multiparous women. White line hernias are painful, small, and difficult to diagnose. Sometimes a diastasis or separation of the rectums is observed, which has no clinical significance. Inguinal hernias are more common in men; indirect ones make their appearance through the pillars of the greater oblique muscle of the abdomen, and may occupy the scrotum.
Auscultation
Formerly, great importance was given to the auscultation of the abdomen, an importance that has been lost in recent years, due to the demonstration of its shortcomings. Thus, pictures of acute appendicitis and strangulated hernias with normal peristalsis are observed; similarly, a silent abdomen does not eliminate the possibility of intestinal obstruction or establish the diagnosis of paralytic ileus. Auscultation precedes palpation and percussion in order to assess peristalsis without stimulating the gastrointestinal tract. To define peristaltic sounds one must have great experience in auscultation of the normal abdomen.
These peristaltic noises can be increased, decreased or abolished.
They are increased in diarrhea and in the early stages of intestinal obstructions.
Loud ringing sounds suggest the presence of intestinal fluid and pressurized air in a dilated intestine, while a succession of these sounds suggests intestinal obstruction. When intestinal contraction occurs during an obstructive condition, the sound will increase in intensity and coincide with manifestations of pain on the part of the patient. In the periods between one access to the other of pain, the abdomen may be silent. Peristaltic sounds are diminished or absent in paralytic ileus and peritonitis. However, remember to listen to the abdomen for five minutes before judging on the absence of bowel sounds. Succussion or punch is obtained by auscultating the abdomen in the epigastric region and shaking the patient from side to side. A characteristic noise will be heard when the viscera, especially the stomach, are filled with fluid. It is seen in pyloric syndrome.
Auscultation may also reveal the presence of abdominal murmurs. There may be systolic murmurs, "venous murmurs," and rubs. Systolic murmurs resemble murmurs of cardiac origin, from which they must be differentiated. They are associated with an arterial obstruction, either at the level of the renal artery, the iliac, the aorta, etc., or the presence of abdominal aortic aneurysms.
The finding of a murmur at the level of the renal artery may have etiological importance in patients with arterial hypertension. Murmurs and rubs can be heard over both hypochondria in tumors of the liver and spleen, and in splenic infarcts. Rubbing in the liver area indicates an inflammatory process of the lining of the organ and is auscultated coinciding with respiratory movements, although they are rare, they can be heard in gonococcal perihepatitis, liver abscess, recent liver biopsy and in liver tumors. In the latter case it is accompanied by a murmur.
Sometimes a soft "venous murmur" is heard at the umbilical level, occupying systole and diastole. Its presence indicates the existence of a portocaval circulation and is virtually diagnostic of portal hypertension.
Fetal sounds can also be heard. Auscultation is performed on the hypogastrium and it is convenient to have a simultaneous arterial reference by palpating the pulse of the radial or femoral artery of the mother. The fetal heartbeat is low-pitched, best heard with the bell of the stethoscope or the wooden stethoscope. Its absence can be used to diagnose the death of the fetus; its increase or decrease may indicate fetal distress or action of drugs ingested by the mother.
 Percussion
Percussion
Percussion alternates with palpation. It is used to demonstrate the presence of liquid, or to determine the size of the viscera, and to differentiate solid masses from liquid masses.
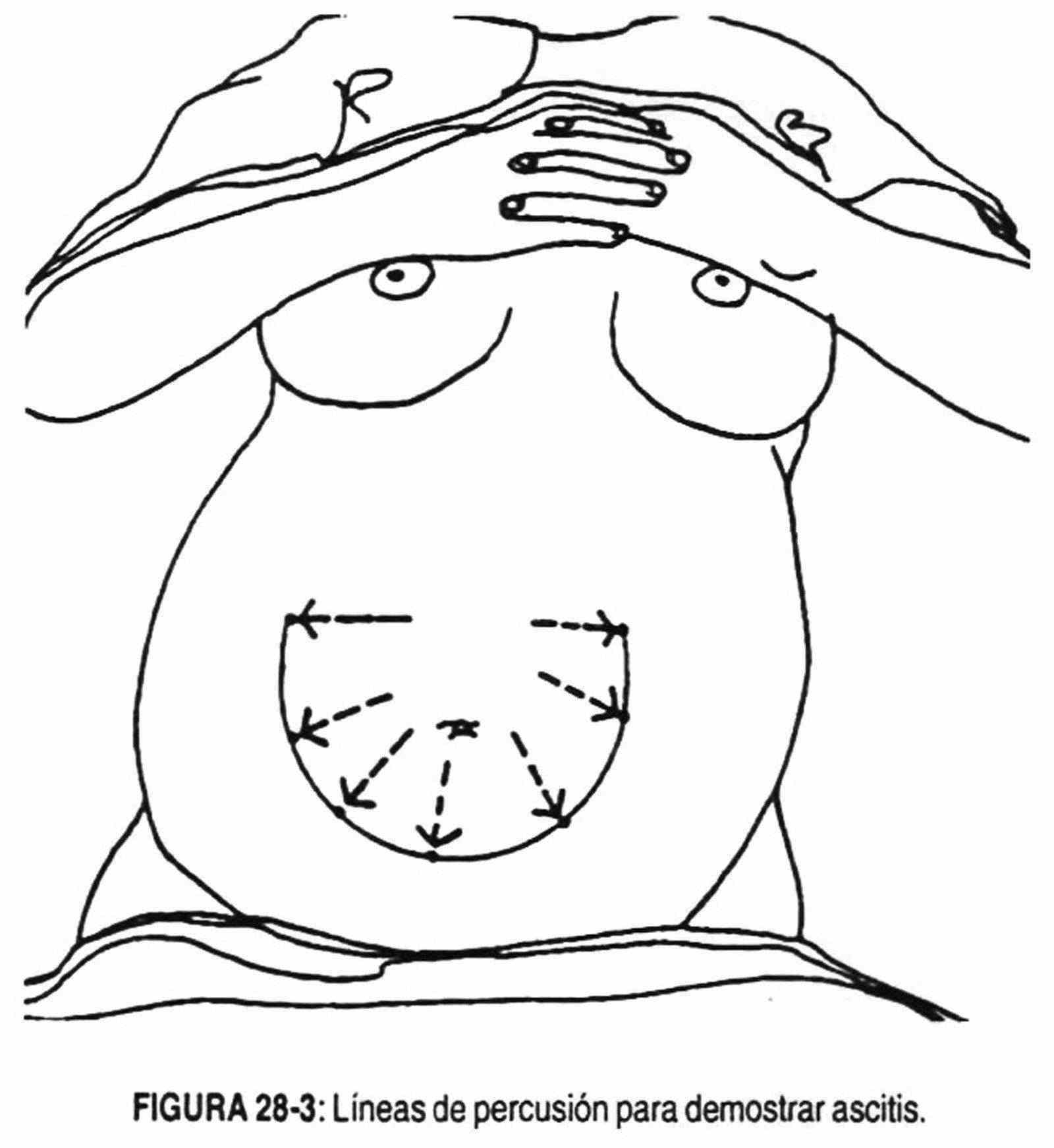
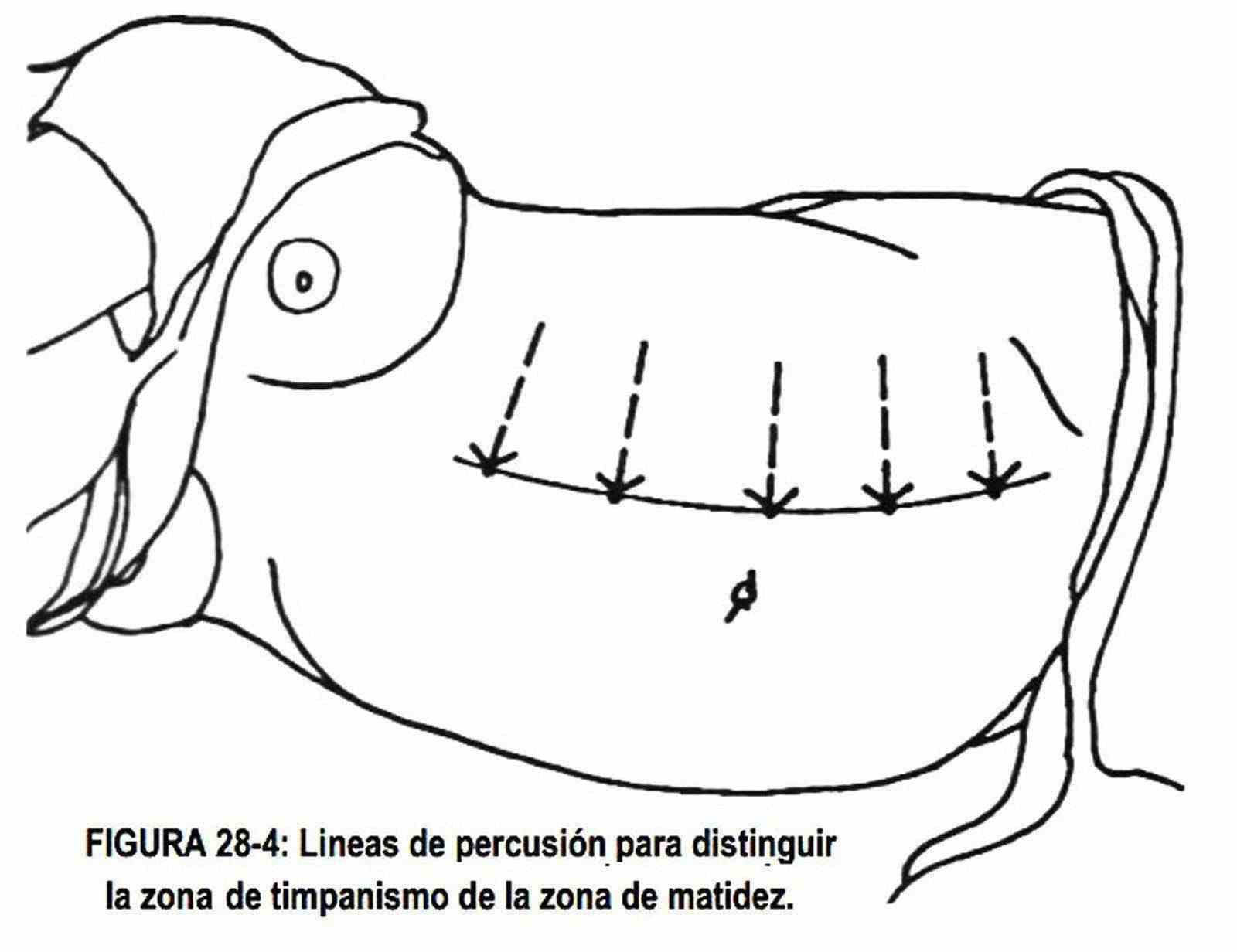
Maneuvers to determine the presence of ascites . The abdomen should be percussed in a radiated fashion (Figure 28-3) from the umbilicus. When there is ascites, a zone of dullness with a superior concavity will be found, at the level of the flanks and the hypogastrium. Using a successive maneuver (Figure 28-4), the presence of ascites can be certified. With the patient in the lateral decubitus position, strike from top to bottom to determine the borderline between bloating and dullness. If the patient has ascites, a marked variation of the line (sign of unevenness) with respect to the line drawn in the previous maneuver will be verified.
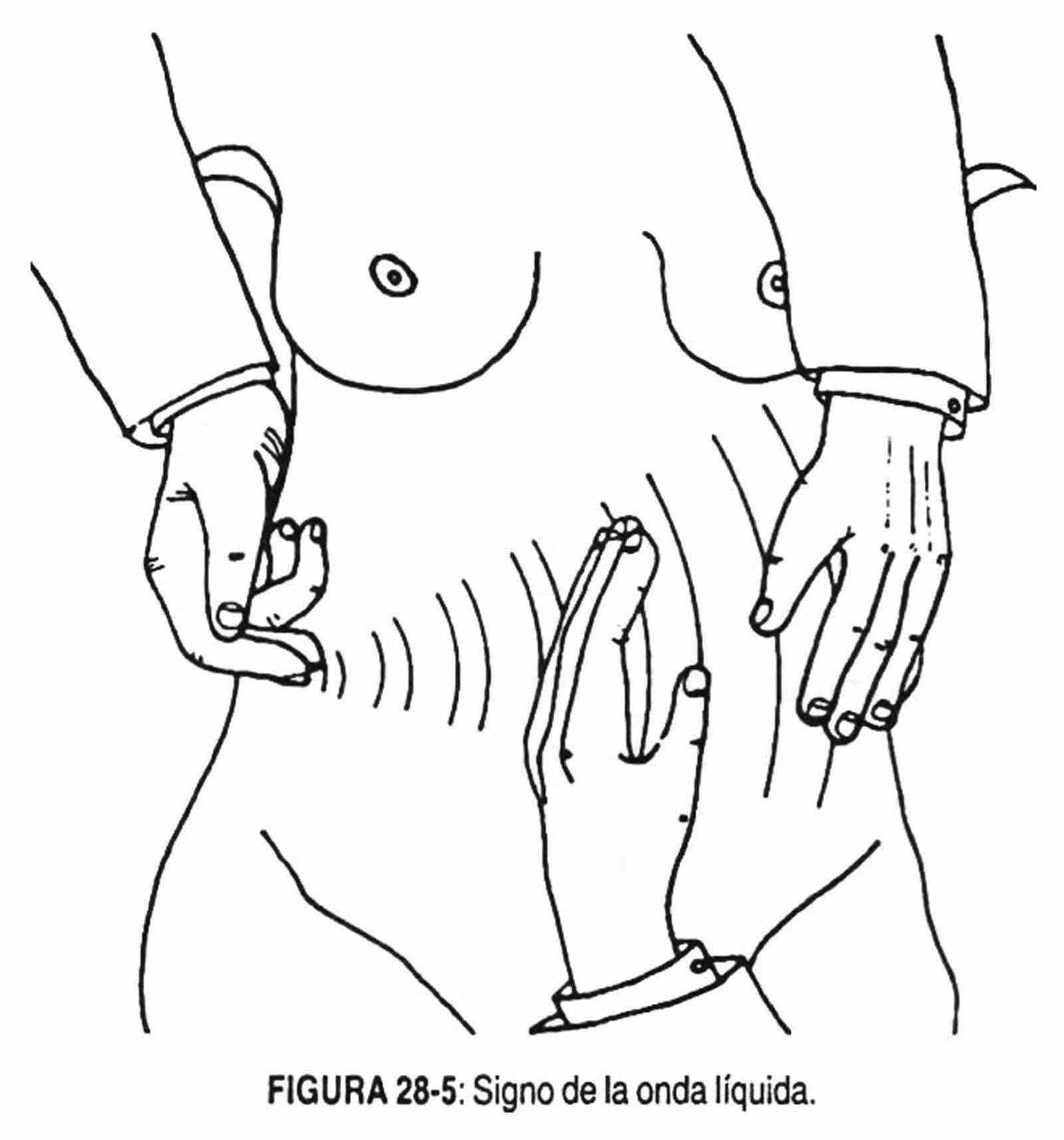
The sign of the liquid wave is sought with both hands. One of them rests on one flank, with the thumb on the infraumbilical zone of the white line or alba. With the other hand, strike on the opposite flank, and if there is ascites, a double blow or double sensation will be perceived in the supported hand. This maneuver can also be performed with the help of a helper who supports the ulnar edge of the hand on the infraumbilical part of the white line (Figure 28-5), replacing the explorer's thumb.
When there is a small amount of ascites (200-300 cm3) the patient should be explored standing up.
 It is percussed from the xiphoid appendix to the pubis, and if there is liquid, a dullness will be obtained in the hypogastrium. The ovarian cyst is differentiated from ascites through percutory maneuvers.
It is percussed from the xiphoid appendix to the pubis, and if there is liquid, a dullness will be obtained in the hypogastrium. The ovarian cyst is differentiated from ascites through percutory maneuvers.
In ascites the line of bloating-dullness is concave upwards, whereas in ovarian cyst this line is convex upwards.
Other findings . Percussion can assess the size of the liver and spleen, and the state of emptiness or fullness of the bladder.
It should be taken into account, when evaluating the size of the liver, that a right pleural effusion can be mistaken for hepatomegaly. A hepatic angle of the colon that is in front of the liver can deceive and make an enlarged liver appear smaller.
Sometimes, between normal lung loudness and normal liver dullness, a tympanic sound is obtained with percussion, due to the presence of air in the abdominal cavity due to rupture of a hollow viscus. This sign acquires importance in acute abdomen pictures.
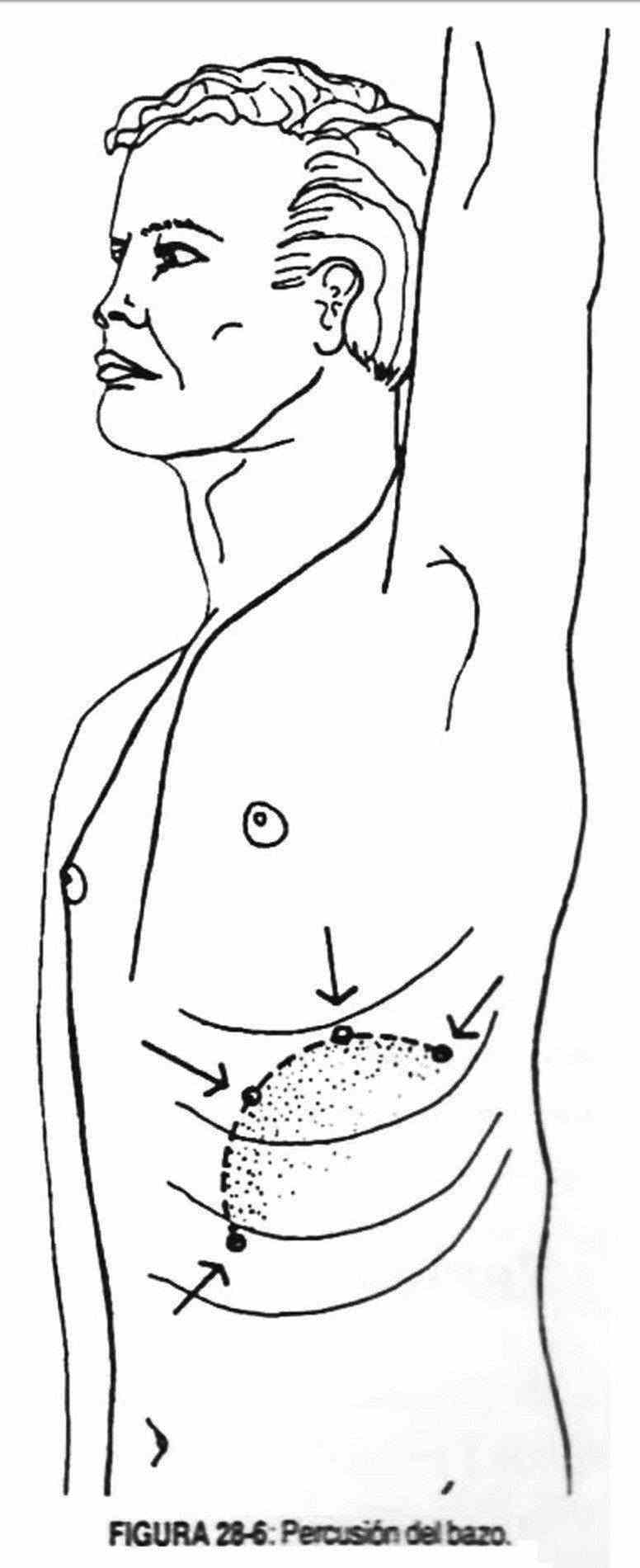
 The spleen is struck in an area at the level of the mid-axillary line in the ninth, tenth, and eleventh intercostal spaces.
The spleen is struck in an area at the level of the mid-axillary line in the ninth, tenth, and eleventh intercostal spaces.
This percussion allows the size of the spleen to be determined. It should not exceed the level of the mid-axillary line in the eleventh costal arch, and it should not reach the anterior axillary line in the ninth and tenth costal arches anteriorly (Figure 28-6).
The urinary bladder can be percussed in the hypogastric region and, when it is distended by the presence of urine, an upward convex upper border will be delimited, which can reach the umbilical region in cases of urinary retention.
In the abdomen distended by intestinal bloating, a generalized tympanic sound will be obtained.
Palpation
Palpation is one of the semiological maneuvers that provides the most information in the physical examination of the abdomen.
At the same time, it will allow corroborating the data collected in the inspection and percussion. Palpation should be performed with gentle and careful maneuvers to avoid rejection of successive examinations by the subject. The usefulness of these maneuvers should be explained to the patient in order to obtain their cooperation. Before starting palpation, you should be asked to cough to increase intra-abdominal pressure and thus delimit a possible painful area.
In this way, abdominal pain caused by abrupt withdrawal of the hand (a sign of decompression) after deep palpation can be avoided in peritoneal irritation. Likewise, abdominal palpation should be initiated in areas away from the painful area. The objectives of palpation are: 1) to look for the presence of pain, 2) to evaluate the characteristics of the abdominal wall, 3) to demonstrate enlargement of the viscera, 4) existence of tumor masses, 5) presence of ascites.
Superficial palpation . In those patients in whom there is a suspicion of an acute abdominal condition, the presence of pain or cutaneous hyperesthesia should be regularly searched for. To do this, the abdominal wall is gently pinched over its entire surface. Cutaneous hyperesthesia is a form of referred pain, produced by visceral or peritoneal irritation or by injury to the abdominal wall.
Superficial palpation is also useful in determining the characteristics of the abdominal wall. The tension of the abdominal wall can be increased, decreased or abolished.
This is determined by probing palpation, i.e., flexing the examining fingers at the level of the proximal metacarpophalangeal and interphalangeal joints.
Wall tension may be increased by increased muscle development. To facilitate relaxation of the abdominal muscles, the patient is asked to bend the knees.
The entire abdomen should be palpated, including the lumbar areas. The patient can be distracted with different maneuvers to differentiate muscular defense from muscular contracture. Muscle defense is produced by tickling, fear of harm, and sometimes by lack of explanation from the doctor to the patient about the maneuvers to perform; it is voluntary and can be overcome simply by talking to the patient and asking him to take conscious deep breaths or bend the knees. Contracture is a secondary reflex, which occurs from an underlying inflammatory process. If there is muscle contracture, the abdomen will remain rigid despite all the distraction maneuvers used.
The contracture and its maximum exponent, the table belly, are produced by peritoneal irritation of the corresponding metamer. The contracture can be located in the region of the affected viscera, or, with the evolution of the disease, become general and produce the aforementioned belly in table.
If an obese patient who has lost weight, or a pregnant woman who has recently given birth, or an abdomen with long-standing ascites is examined, palpation will detect muscle hypotonia.
 In acute abdomen or peritoneal irritation, look for the sign of decompression, which consists of withdrawing the hand after having deepened it; in the positive case there is pain that the patient places in the place of the inflamed viscus. This sign has its origin in peritoneal traction induced by sudden movement. As already mentioned, there are less aggressive maneuvers to assess the possibility of peritoneal irritation, such as asking the patient to cough or push.
In acute abdomen or peritoneal irritation, look for the sign of decompression, which consists of withdrawing the hand after having deepened it; in the positive case there is pain that the patient places in the place of the inflamed viscus. This sign has its origin in peritoneal traction induced by sudden movement. As already mentioned, there are less aggressive maneuvers to assess the possibility of peritoneal irritation, such as asking the patient to cough or push.
Another maneuver to take into account in superficial palpation of the abdomen is that used to differentiate a tumor in the wall from a tumor in the abdominal cavity.
For this purpose, the patient is asked to flex his head or raise his feet, thereby increasing the tension of the abdominal wall muscles. If the mass is abdominal it will disappear with this maneuver, and if it is part of the wall, it will continue to be palpated despite muscle contraction, or it will become more evident.
Painful spots or areas in the abdomen
The pain can be caused by inflammation of the superficial tissues or abdominal viscera.
To differentiate one from the other, the same maneuver used to distinguish abdominal wall masses from deep abdominal masses is used. This is achieved, while the painful area is palpated, by asking the patient to flex the head or raise the feet. If the pain is superficial it remains unchanged or increases; On the other hand, it disappears if it originates in the viscera of the abdomen.
In turn, the pain can be referred to the abdomen from thoracic pathologies, such as acute lung disease, or from pelvic inflammatory disease. Sometimes these pictures can be accompanied by pain on decompression and wall stiffness.
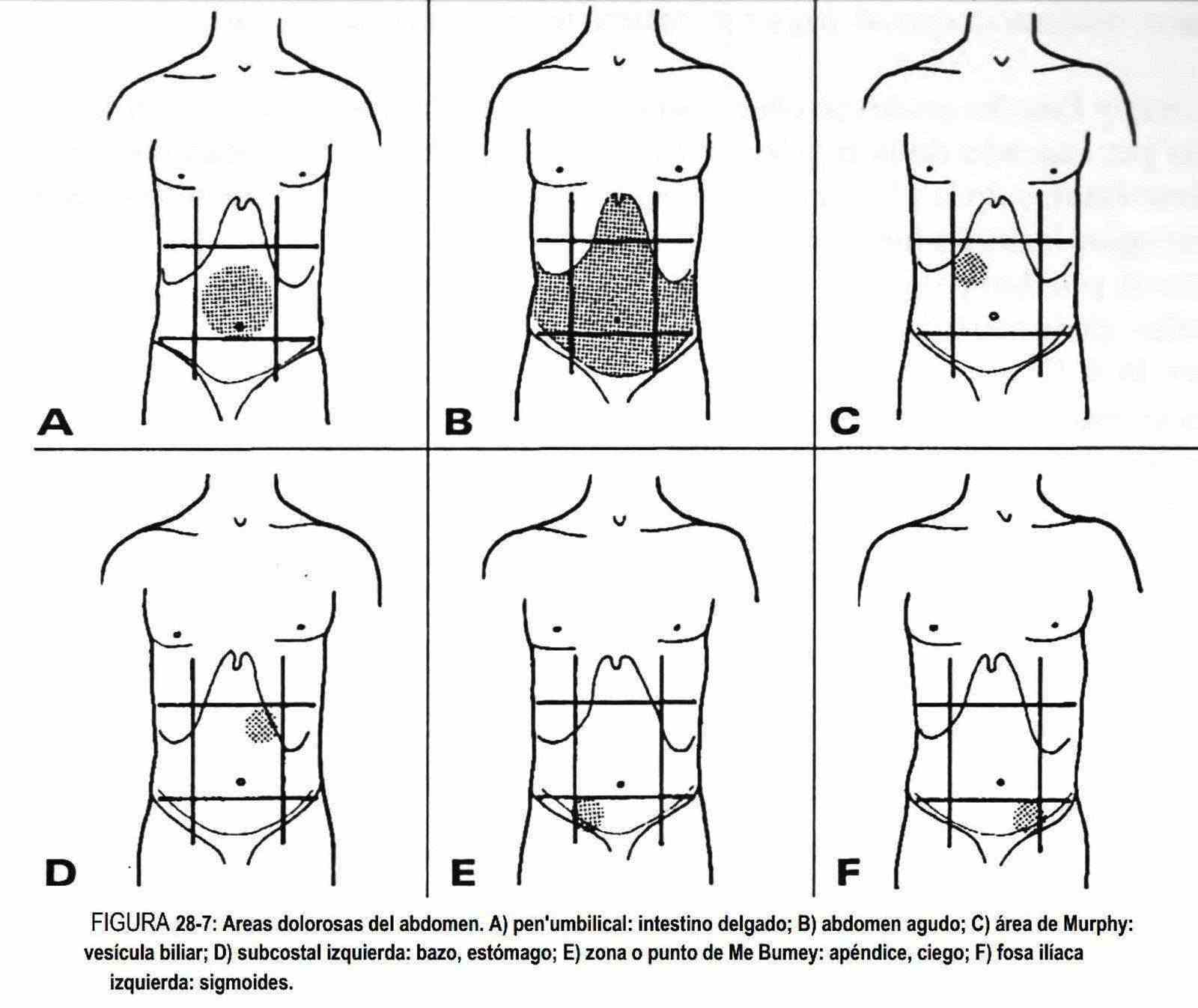
Normally, palpation of the aorta, liver, cecum, and sigmoid can be slightly painful. Classically, pain produced by palpation with the index and / or greater finger on the external border of the rectus abdominis in the subcostal region, especially in deep inspiration, is described as characteristic of inflammatory gallbladder disease.
When in this case the pain interrupts the respiratory movement, it is the so-called Murphy's sign.
In the middle of the line that joins the umbilicus with the anterior superior iliac spine is the McBumey point or appendicular pain point. If the intersection of the external border of the anterior rectus of the abdomen with the horizontal of the navel is sought, there will be found the upper painful point of the ureter, and at the junction of the external third with the internal two thirds of the biliac line, the ureteral point will be found means, medium. The lower ureteral point is sought during the digital rectal examination.
On the posterior wall of the abdomen, the point where the last costal arch joins with the outer edge of the costovertebral muscle mass (costovertebral point) should be pressed, which topographically corresponds to the area where the kidney is close to the skin surface. It is painful in diseases of the renal parenchyma, although it sometimes hurts in acute pancreatitis and retrocecal appendicitis. In addition, the lumbar fossa should be percussed with the ulnar edge of the fist for pain (Figure 10-6). Normally the patient may report an unpleasant but not painful sensation. In case of inflammation, infection or kidney stones, this fist percussion will cause pain, which is why the maneuver must be performed gently and carefully.
Deep palpation
Once the superficial palpation is finished, and if the conditions of wall tension allow it, the deep palpation begins. If there is pain, the areas furthest away from it are palpated, explaining to the patient the importance of each maneuver. When necessary, percussion will accompany palpation to delineate and compare size and consistency.
Liver . The liver is palpable when it is increased in size or consistency; the enlargement of the liver is called hepatomegaly. On other occasions, and without hepatomegaly, the liver can be palpated in thin subjects due to lack of subcutaneous cellular tissue, or in tilted or lowered livers due to emphysema or subphrenic abscess. It is rarely palpable in normal subjects. In normal children, the hepatic margin is often palpable, one to two centimeters below the costal margin. The child's liver will be diseased when it exceeds two centimeters from the costal margin and is increased in consistency.
The size of the liver must be defined not only by palpation but also by percussion.
This last maneuver will delimit the upper level of the organ. Under normal conditions, from upper limit to lower edge should not exceed ten centimeters. The size of the liver should be reported by the number of centimeters below the costal margin, and in turn by the number of centimeters measured from the upper to the lower limit. The dome of the liver is in the fifth costal arch at the level of the hemiclavicular line. It may be lowered in asthenic subjects. Under normal conditions it moves with respiratory movements.
In longilinear subjects, the liver may be elongated, and the right lobe tends to be directed toward the iliac crest, and under these conditions it is normal to be palpable. The liver can increase in size due to the accumulation or infiltration of fat, glycogen, glycosides, iron, amyloid, leukemic or lymphomatous cells, due to biliary obstruction, venous congestion due to heart failure, inflammatory congestion (hepatitis), liver cirrhosis, and in tumors benign and malignant, primary or secondary. The causes of palpable liver are listed in Table 28-1.
|
Table 28-1 Causes of palpable liver |
|
The lower border of the liver will be blunt or sharp according to the variations in liver volume. This edge may be smooth or irregular. In venous congestion of the liver it will be blunt and smooth, and it will be sharp and irregular in some cirrhosis of the liver; in the metastatic liver it may be felt irregularly.
The liver surface is palpable by deep scanning, and may be regular or irregular. Tracing is a deep palpation performed by sliding the hand over the palpated area. It will be seen to be irregular or embossed in macronodular cirrhosis, metastatic livers, and primitive tumors.
The consistency of the liver is perceived during palpation of the lower border, at the moment when the fingers receive this border. It can be gently compressed to feel its elasticity. The consistency can be soft-elastic as seen in hepatitis, fibroelastic as occurs in infiltrated livers, and stone as occurs in tumor livers.
Palpation of the liver may be painful or painless. It will arouse pain in hepatitis, in the congestive liver of heart failure and in primitive liver tumors.
Spleen . The spleen should not normally be palpated. Before a palpable spleen becomes conspicuous, there is an increased area of dullness. Hence the importance of perceiving the splenic area.
Splenomegaly is any enlargement of the spleen and should be reported in centimeters below the costal margin. The larger the size of the spleen, the closer it will be to the umbilical line; grows along the line of the arch of the fifth and tenth ribs. What is palpable is the lower pole of the organ, and sometimes also the notch. The spleen is an organ that is palpable superficially, unlike the liver. The consistency of the spleen is increased in hyperplastic, congestive or infiltrative processes, especially in those long-standing splenomegaly.
There are some painful splenomegalies, as they occur in acute hyperplasia, for example, in bacterial endocarditis and infectious mononucleosis, and in splenic infarcts.
In children, the spleen is often palpated within a centimeter of the costal margin, soft, painless, and without pathological significance.
Large spleens may have lumbar contact and have balling; Unlike the kidney, the spleen has greater respiratory mobility.
Kidney . Normally, the right kidney can be palpated at the level of the corresponding flank.
The finding of a kidney out of its usual place means that the organ has descended; it is known by the name of renal ptosis. It occurs due to laxity of the perirenal connective tissue or due to its weight gain due to the presence of tumors or cysts. Other times, the kidneys may be palpated because of congenital malformations, such as a horseshoe kidney.
The normal shape of the kidney can be lost and take on different irregular characteristics produced by different congenital anomalies, as occurs in the horseshoe kidney and in the renal ectopy, in which the two kidneys are on the same side. The shape can also be altered by the presence of cysts and / or tumors.
The size is increased in hydronephrosis, polycystic kidney, tumors, and abscesses.
The surface can be smooth or embossed, when there are cysts or tumors, while the consistency is increased in tumors. Regarding kidney sensitivity, its palpation can be painful, for example, in some acute infectious processes such as abscesses and pyelonephritis; and in these cases the fist percussion is positive.
Urinary bladder and other pelvic organs . The urinary bladder is usually not palpable.
When there is a urethral obstruction or with distension of the same, the bladder can be palpated in the hypogastrium, smooth, borderless and painful, and palpation increases the desire to void. The percussion helps to delimit it, finding a convex edge upwards. In the hypogastrium, an enlarged pregnancy uterus, hydatidiform mole, choriocarcinoma, and fibromas can be palpated. An ectopic pregnancy, ovarian or soft tissue masses, or ovaries that are enlarged due to endometriosis may also be palpated. The gynecological examination will help to differentiate these pictures from other intra-abdominal pathology.
Cecum and sigmoid colon . The cecum and sigmoid colon are palpable in the healthy subject. Fermentative dyspepsia or indigestion is accompanied by a distended cecum, with air-fluid noises and tenderness. If there is acute inflammation, diverticulitis, or appendicitis, palpation is painful. There will be pain upon decompression, and eventually contracture in the area of the inflamed viscus, which may generalize to the entire abdomen when the infectious process spreads to the peritoneum. In this situation, cutaneous hyperalgesia can be observed.
When the decompression maneuver is performed, the pain can be referred to the site of the inflamed viscus. Thus, pain upon decompression of the left iliac fossa can refer to the right iliac fossa in appendicitis, and to the left iliac fossa when the right iliac fossa is decompressed in diverticulitis.
Psoas and obturator signs are sometimes found in acute appendicitis. The psoas sign consists of the appearance of pain when the right iliac fossa is compressed while flexing the hip with the right lower limb extended. The obturator sign is the appearance of pain when flexing the right knee and hip together with the rotation of the lower limb, and is due to irritation of the obturator muscle in inflammatory conditions of the right iliac fossa.
Gallbladder . Normally, the gallbladder is not palpable, but it can be when it is enlarged by obstructive lithiasic or tumor processes. In acute cholecystitis, palpation of the area is painful.
Occasionally, the gallbladder is palpated in the right upper quadrant with a rounded or piriform shape, of elastic, reluctant or fluctuating consistency, and of variable size depending on the degree of distension, painful or not; this, added to jaundice and acholia, constitutes the so-called Courvoisier-Terrier syndrome, observable in neoplasms of the head of the pancreas and in choledochal lithiases.
The gallbladder can be mobilized laterally or pendulously, and it also moves with respiration.
On rare occasions, he has lumbar contact and has rally; lacks palpable borders.
Upper abdomen . On palpation of the epigastrium, the presence of an expanding pulsatile tumor suggests an aneurysmal dilation of the aorta. In the case of tumors that have contact with the great vessels, throbbing may occur, but not expansion. At this time, auscultation should be performed in search of murmurs and / or rubs typical of vascular anomalies.
 Finding of tumor masses . On palpation of the abdomen, a mass or tumor may be found, which must first be defined in terms of its topographic location. The topographic location will guide, according to anatomical knowledge, on the possible origin of the tumor; it may be part of a viscera, or be in contact with it or not have any relationship with an abdominal organ.
Finding of tumor masses . On palpation of the abdomen, a mass or tumor may be found, which must first be defined in terms of its topographic location. The topographic location will guide, according to anatomical knowledge, on the possible origin of the tumor; it may be part of a viscera, or be in contact with it or not have any relationship with an abdominal organ.
In relation to the superficial muscular plane, it must be demonstrated whether the tumor mass is in the anterior wall or in the abdominal cavity. To do this, the patient will be asked to flex the head or lift the feet, in order to contract the abdominal muscles. Whether the mass belongs to the wall will remain unchanged or will become more apparent. However, it will disappear if it is located in the peritoneal cavity.
Often it is not easy to completely delimit a tumor mass, especially in globular abdomens, with developed muscular walls or with ascites. Therefore, it is important to carefully and orderly palpate the abdominal viscera in order to be able to describe the palpated mass well. The shape, the size in centimeters, the limits (if they are clear or diffuse), the surface, the consistency (if it is soft, elastic, fibrous or stone), the respiratory mobility and palpation, lumbar contact and the presence or absence of heartbeats (which should be immediately auscultated) and pain.
Form . The shape of the palpated tumor will be described based on its semiological characteristics. It should be said rounded, ovoid, piriform, irregular, avoiding comparison with known structures (orange, etc.).
Size . It will be described in centimeters of length, width and depth. It is convenient that the doctor knows the size of your hands and fingers to compare them with the tumor found.
Limits . They are neat when clearly differentiated from neighboring structures and diffuse when they cannot be distinguished from adjacent organs.
Surface . It can be smooth or without relief, and irregular or with relief, sometimes embossed.
The irregularity may or may not be uniform, and the reliefs found of the same or different size. They may or may not have a tendency to converge as well.
Consistency . It can vary from soft to stony, with different levels in between.
It will be soft when it is similar to the consistency of the abdominal wall. If a mass with liquid content is palpated, it will be tender when the liquid fills the mass, and fluctuating when it does not produce tension in the wall.
The consistency is elastic when the shape of the mass varies with palpation, and in this sense the most characteristic example is palpation of a muscle mass.
There is talk of a fibrous consistency when it is hard and its shape does not change, and a stony consistency when the hardness is extreme.
Sensitivity . It should be indicated if the mass is painful or not on palpation.
Mobility . Mobility is described in relation to the manual movements made by the explorer; with breathing, usually in muscular structures of the upper abdomen; if it beats and / or expands; if you have mobility related to the digestive tract, classically called a phantom tumor (localized meteorism due to incomplete intestinal obstruction).
Temperature . It will be described in superficial or wall tumors. Finally, maneuvers must be performed to define the relationships of the tumor mass with the superficial and deep planes.
All these qualities will guide the probable origin of the tumor.
Thus, for example, a pancreatic cyst, a soft tissue sarcoma, a renal cyst or a cecum tumor can be examples of the above.
It is also possible to perform a preoperative general anesthesia and then repeat the in-depth examination of the tumor masses. Likewise, anesthesia can be used to search for tumors by bimanual palpation, which combines abdominal palpation with rectal or vaginal examination.
Ascites . The maneuvers to demonstrate the presence of ascites have already been described in the paragraph on percussion. Occasionally, by deepening the hand over the right upper quadrant, fluid displacement is perceived and then collides with the liver. It is the so-called iceberg sign. The rise of the liver is sometimes palpable in ascites, like a second shock.
Rectal examination
 Every man over the age of forty should have a rectal exam every year; it is a source of information in relation to an area that is difficult to access by other exploratory techniques.
Every man over the age of forty should have a rectal exam every year; it is a source of information in relation to an area that is difficult to access by other exploratory techniques.
In prolonged febrile syndromes due to the presence of prostatitis or periprostatic abscesses, in patients with bone pain and in patients with rectal bleeding or anal discomfort, a rectal examination is essential. Sensitivity and specificity exceed ultrasound.
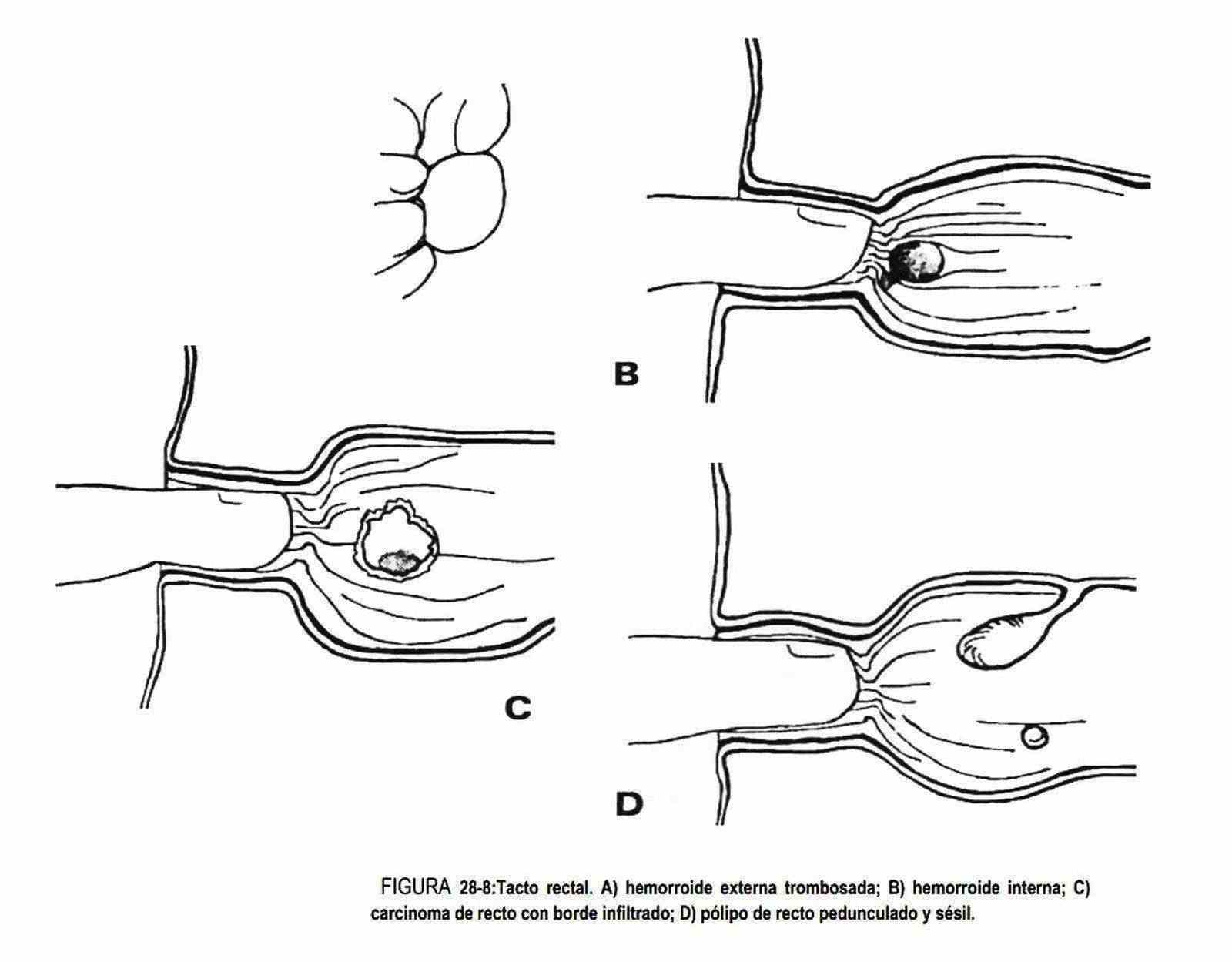
The decreased tone of the anal sphincter can be verified in elderly patients, in different congenital anomalies, in myelomeningocele or after surgical procedures in the area. There may be increased tone due to infection, inflammation of the rectal area, or it may be absent in lower neurological lesions. Hemorrhoids can also be detected, seen as bluish cords below the anorectal line. They are red and swollen when thrombosed (Figure 28-8, A). The digital rectal examination will produce pain in cases of perirectal abscesses. Other times, a decrease in the rectal mucosa or prolapse will be observed; sometimes it is necessary for the patient to perform a Valsalva maneuver to highlight it.
Anal fissures and fistulas are easily seen before digital rectal examination. Scratching excoriations of the anal region can be found in patients with itching due to intestinal parasitosis, and fungal lesions, dermatitis, chancre, warts, herpetic lesions and condylomata acuminata are also described on the skin of the anus.
Rectal, pedunculated, or sessile polyps (Figure 28-8, D), adenopathies, metastatic tumors in the rectal peritoneum (cassette sign) can also be palpated. Fifty percent of rectal tumors develop in an area within reach of the examining finger (Figure 28-8, C). When removing the finger, the examiner should look for blood or perform the occult blood test and observe the characteristics of the stool.
In peculiar situations, foreign bodies may be found. The prostate should always be palpated. In cases of prostate cancer, it will be played larger than normal, with increased consistency (which can become stony), loss of its normal, fixed and irregular shape, and even the disappearance of its limits. Benign prosthetic hypertrophy is very common in men over fifty years of age. It tends to erase the middle sulcus, it is symmetrical and painless, of elastic consistency, and with an upper limit that is difficult to palpate. On other occasions, the prostate is perceived to be of increased consistency, painful and with areas of fibrosis; This corresponds to chronic prostatitis, although it is difficult to diagnose by digital rectal examination. Acute prostatitis are very painful and in them the consistency and temperature are increased; in these cases,
Sacrococcygeal or pilonidal cysts are congenital and are found in the midline at the sacrococcygeal level. They frequently drain a secretion that is scanty and can be complicated by fistulas and abscesses.