by Alberto J. Muniagurria and Eduardo Baravalle
Physical examination of the chest includes examination of the skin, musculoskeletal and joint structures, and examination of the breasts (Chapter 27) and the respiratory and cardiovascular systems (Chapter 26).
Examination of the chest is performed by inspection, palpation, percussion, and auscultation.
THORACIC WALL
Skin
Abnormal findings of the skin of the chest do not differ from abnormal findings of the skin in general. Arachnid nevi can be found on the skin of the thorax, which can be seen as spider veins consisting of a central point from which new vessels originate, and which disappear with vitro pressure. This finding is characteristic of chronic liver diseases, and occasionally appears during estrogen treatment. On other occasions, following the course of the intercostal nerves, vesicles with stellar borders are found on an erythematous area, with intense itching and pain, typical of herpes zoster.
Palpation of the thoracic skin may reveal the presence of air in the subcutaneous cellular tissue; this is evidenced by crackles and is seen in some patients with pneumothorax and pneumoperitoneum.
Articular and musculoskeletal system
At the thoracic level are the chondrocostal and chondrosternal joints and the sternocostoclavicular joint. These joints can be the seat of inflammatory processes, with pain on superficial and / or deep palpation. When the sternocostoclavicular joint is affected, a painful condition known as Tietze's syndrome occurs, it must be differentiated from other chest pain. If there is pain on palpation in one or more rib arches, rib fissures or fractures should be suspected.
Hypertrophy of accessory respiratory muscles is seen in patients with chronic respiratory failure. Sometimes there is a decrease in muscle masses, constituting muscle atrophies (neuritis, poliomyelitis, etc.).
Abnormal forms of the thorax
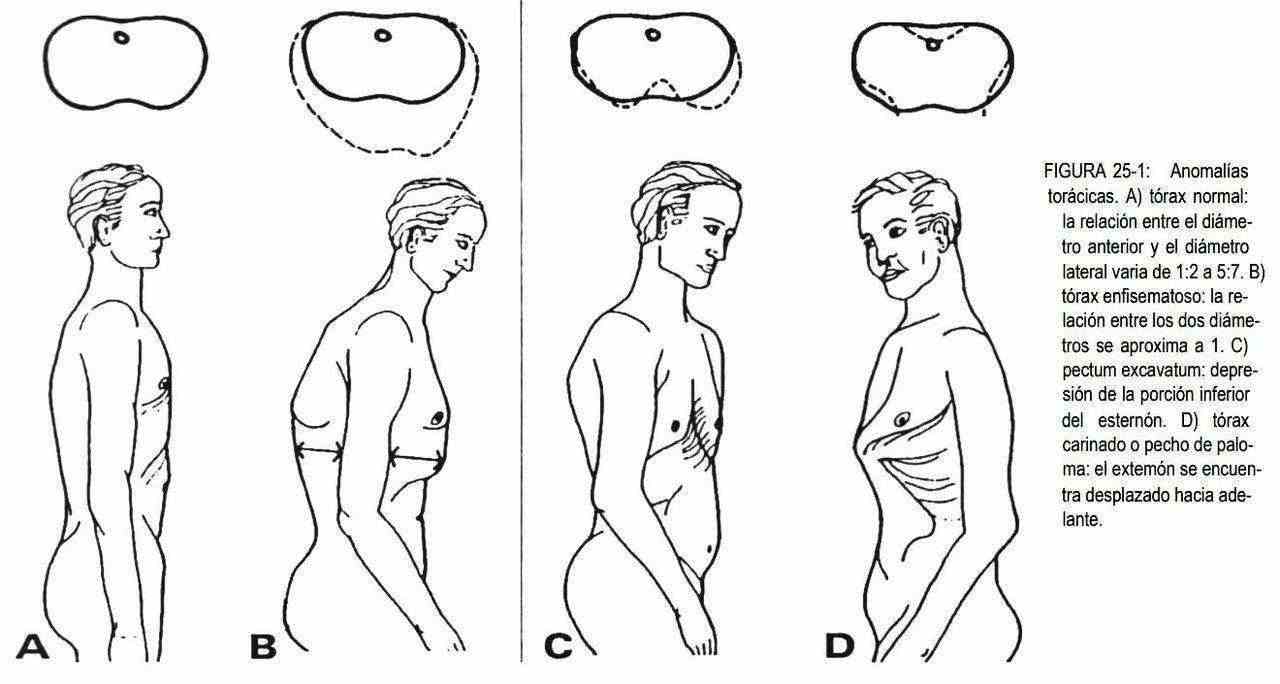
Normally, there is no perfect thoracic symmetry, due to the greater muscular development of a half body (for example, the right in right-handers) or to small variations induced by habit. Under normal conditions, the ratio of the anteroposterior diameter of the thorax to the lateral diameter ranges from 1: 2 to 5: 7 (Figure 25-1, A). When this ratio approaches 1, the chest will be barrel or barrel-shaped, which is observed in the elderly and in patients with chronic obstructive pulmonary diseases (Figure 25-1, B) when there is depression of the sternum and the diameter anteroposterior decreases, we speak of pectum excavatum (Figure 25-1, C), a malformation that can be associated with Marfan syndrome, mitral valve prolapse, and straight back syndrome.
The thorax may present asymmetries in patients who have undergone pneumonectomies or thoracoplasties and in patients with deformities in the thoracic spine. These deformities include kyphosis, scoliosis, and lordosis. Kyphosis is an exaggeration of the normal curvature of the thoracic spine (Figure 25-2, B). It is possible to observe it in the elderly, forming an anterior concavity curve, due to the decrease in height in the anterior part of the vertebral bodies, and also in subjects with osteoporosis and in patients with vertebral tuberculosis.
Thoracic lordosis is a less frequent malformation of anterior convexity, which can present as compensation for kyphosis in patients with weak spinal muscles and excess abdominal weight.
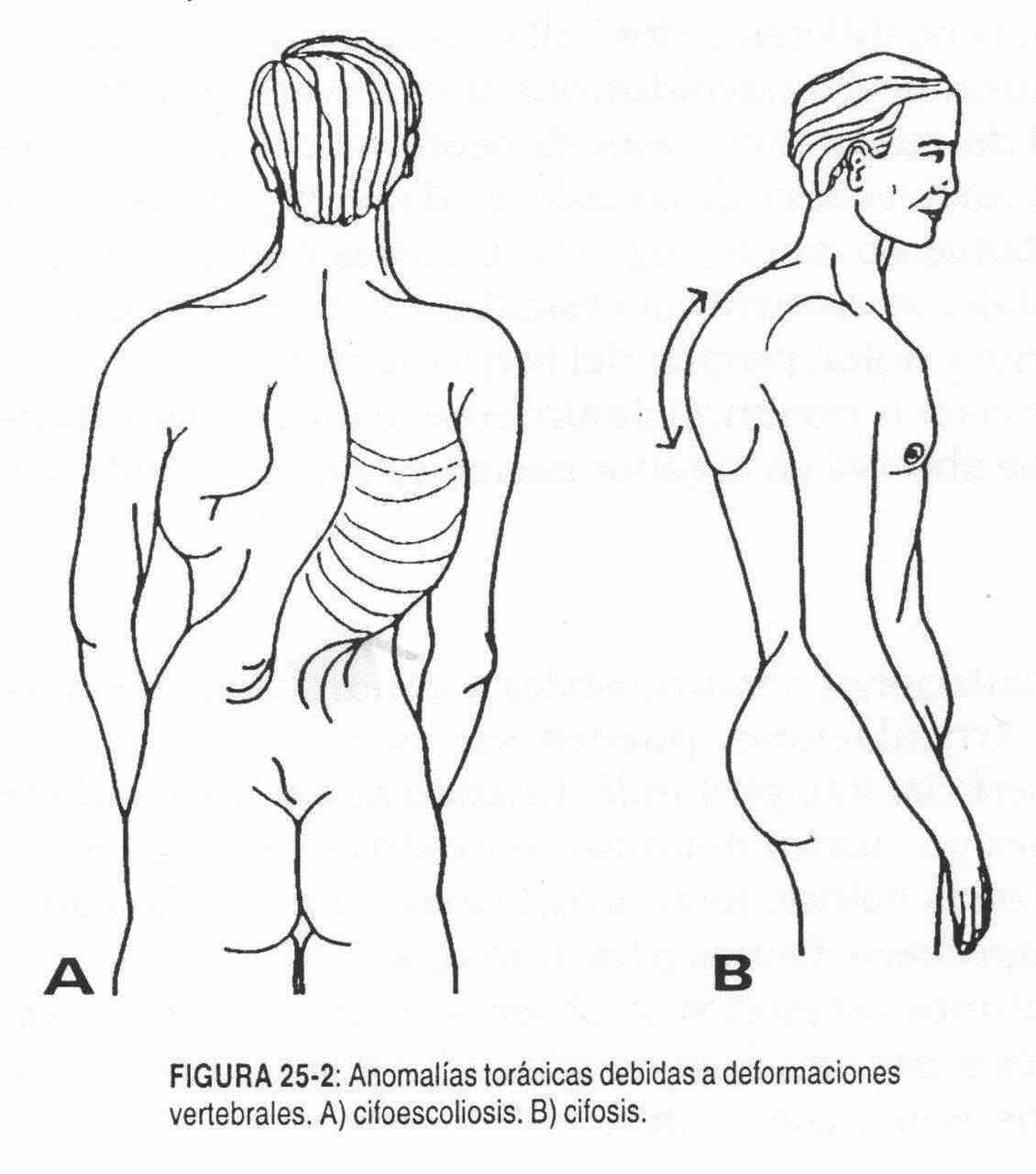 The thoracic spine may also have a left or right concavity curve, which, if combined with kyphosis, leads to kyphoscoliosis (Figure 25-2, A).
The thoracic spine may also have a left or right concavity curve, which, if combined with kyphosis, leads to kyphoscoliosis (Figure 25-2, A).
The most common cause is abnormal development of the vertebral bodies, which are also rotated.
RESPIRATORY APPARATUS
Inspection
Respiratory rate and rhythm, already described in the chapter on vital signs, are first evaluated. The rate may be increased (tachypnea) or decreased (bradypnea).
The rhythm may be disturbed, and irregular rhythms such as Cheynes-Stokes and Biot are occasionally observed (see Chapter 16). The longest duration of expiration relative to inspiration can be found in abnormal situations.
The intercostal spaces sometimes retract on inspiration or protrude on expiration, this phenomenon is called pulling and can be observed in chronic obstructive pulmonary diseases and in patients with respiratory failure. These patients may also have nasal flaring and lip closure during exhalation (trumpeter's mouth).
In certain cases, inspection allows a localized decrease in respiratory movements to be observed. This fact suggests the presence of disease of the pleura or of the underlying lung tissue.
Palpation
Respiratory mobility may be globally or locally reduced, suggesting the existence of pleural or lung disease, or musculoskeletal diseases.
The vowel thrill may be increased, decreased, or abolished. It will be increased in pulmonary condensations with patent bronchus (eg, acute lung disease) or in pulmonary condensation that can occur above a pleural effusion, with patent bronchus, and whenever this condensation is in contact with the chest wall. The vocal thrill will be diminished or abolished when there is a decrease in voice intensity, in bronchial obstruction, in pleural effusions and pneumothorax, and if there is interposition of solid tissue between the lung and the palpatory surface.
On certain occasions, with the hand on the rib cage, a rasping palpatory sensation can be picked up, which corresponds to a pleural rub. This occurs in patients with pleural inflammation without effusion, is accompanied by pain, does not disappear with coughing, and increases with hand pressure.
Percussion
Percussion should begin at the site furthest from where an injury is suspected.
Under abnormal conditions, instead of normal loudness, dullness, submatidity, hypersonousness, and bloat may appear in the chest. Dullness is found in pulmonary condensations, with patent bronchus or not, and in pleural effusions. In the latter case, and when there is a mobile pleural effusion, changes in the patient's position will cause the dullness to shift towards the place of greatest decline. It is the so-called sign of the unevenness. Hypersonority is detected in patients with pneumothorax and in emphysematous subjects. When the pneumothorax is under tension it is possible to obtain a tympanic sound. Localized areas of hypersonority can also be found in patients with solitary bullae.
Auscultation
The respiratory sound auscultated at the level of the thoracic wall can be, in pathological situations, diminished or absent.
It is diminished or absent when there is a great difference in the vibratory properties from the place of origin of the sound to the thoracic wall. This is how it can be reduced in obese subjects, in which the adipose tissue filters the respiratory sound. Similarly, the interposition of fluids or air (pleural effusion or pneumothorax, respectively) in the pleural cavity also produces a decrease or absence of respiratory sound. In patients with emphysema, the lung tissue is hyperinflated, which modifies its acoustic properties and hinders the transmission of sound between the over-distended lung tissue and the chest wall.
In addition, in the emphysematous lung the bronchial noise is softer or weaker, thus contributing to the decrease in respiratory sound. In primary emphysema, bronchial compression occurs due to the loss of elastic tension in the lung; thus, the air flow in the large bronchi is normal. In the mouth, the inspiratory flow is silent, with an extremely affected expiratory flow.
In contrast, in chronic bronchitis and asthma, the inspiratory flow at the level of the mouth is noisy.
When there is obstruction of a bronchus, at that level bronchial noise is not generated. In pulmonary atelectasis, or pulmonary consolidation produced by the obstruction of this bronchus, no respiratory sound will be heard in the part of the chest corresponding to the obstructed segment.
In cases of bronchial stenosis, as in asthma and chronic bronchitis, there is greater turbulence that generates an increase in the auscultated respiratory sound. In asthma, the obstruction is not uniform, and is characterized by changes in the caliber of the bronchi with great regional variation. The sound of severely constricted bronchi contributes more than is due to the production of respiratory sound, which explains the existence of areas with increased respiratory sound.
In chronic bronchitis, where the obstruction is uniform throughout the lung, no large differences are found in the intensity of the respiratory sound.
Bronchial sound
On certain occasions, the turbulence generated at the level of the large bronchi (bronchial sound) can be heard as such in the chest wall, replacing the vesicular murmur or normal respiratory sound is known as main noise, this sound auscultated with the stethoscope is the The same as that normally heard at the level of the trachea and in the sternal area, and it retains the characteristics of high frequency, blowing respiration and being auscultated on inspiration and expiration. This occurs when there is a lung consolidation with a patent bronchus, as seen, for example, in pneumonia and atelectasis with a patent bronchus. It is important to emphasize that the bronchus producing the turbulence must not be obstructed.
Added noise
Regarding lung sounds, numerous terms have been used to name the pathological phenomena of the lung parenchyma. These names, which acknowledge their origin in the terminology used by Laennec, have suffered from overlap and confusion, and led to a lack of clarity in describing precise anatomical facts.
In recent years, these terms have been rethought, trying to classify them with a new name.
Both explosive noises and musical noises were originally called "rales" or "rales", a term that emerged from the gurgling heard in the dying patient.
There was also talk of adventitious sounds that could be mucous, wet and hissing. The name crackling was used for those supposedly dry noises and subcrepitation to explain the presence of secretions in the fine airway. An attempt was made to classify the aggregated sounds according to the bronchial lumen into fine, medium and thick bubble sounds.
These aggregate or pathological noises were progressively divided into rhonchi and rales, with low-frequency musical sounds being called rhonchi, and non-musical short-duration explosive noises rales.
From the analysis of acoustic terms and their correlation with physiological facts, Paul Forgacs proposed, in 1957, to use the Robertson and Coope classification.
These authors classified the added noises as "wheezes" or continuous sounds and "crackles" or interrupted sounds. The continuous or musical sounds or "wheezes" were classified, according to their tone in rhonchi if the tone is low and wheezes if it is high; for its duration in long and short; by the location in the respiratory cycle in inspiratory and expiratory; and taking into account its complexity in monophonic and polyphonic.
The "crackles" or interrupted sounds are explosive noises, not musical, which are classified by their number as isolated or profuse; by its location in the respiratory cycle in inspiratory and expiratory; if they are soft, very short and high-pitched they are called crackles or fine, and if they are more intense, somewhat less short and low-pitched, they are called sub-crackles or coarse.
In our environment, due to semantic difficulties, it is difficult to understand that rhonchi, sounds directly related to bronchial secretions, are classified as a hissing or "wheeze" sound. The reason is that the term "wheeze", when translated, is associated with a hissing sound, when in fact it refers to a continuous sound, which can be graphed as a straight line.
 Continuous sounds or "wheezes" (rhonchi and wheezing)
Continuous sounds or "wheezes" (rhonchi and wheezing)
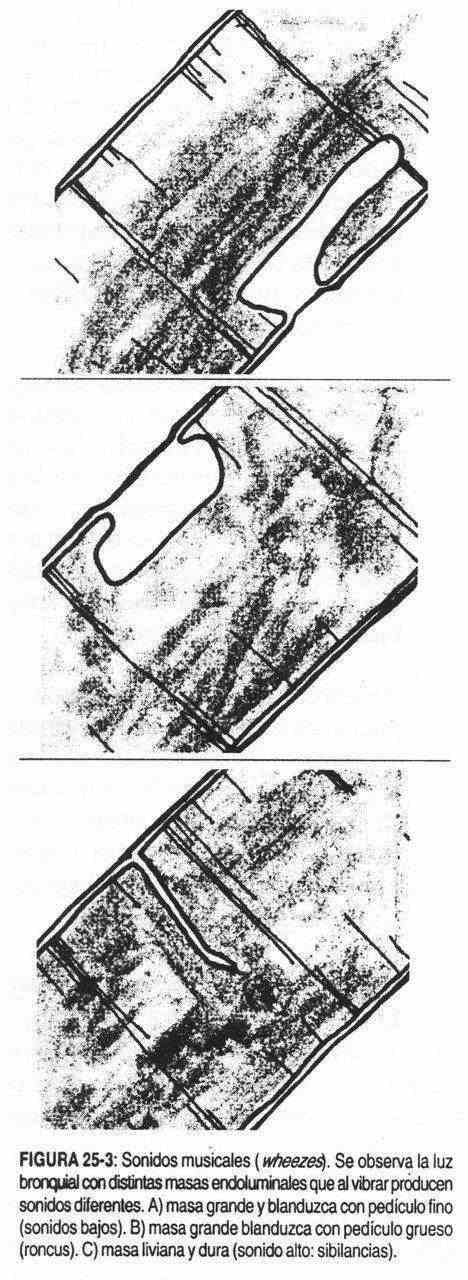
It was always believed that the lung produced continuous, musical sounds or "wheezes" by a mechanism similar to that of a wind instrument. The instrument that most closely resembles a model is the children's trumpet. These trumpets can only give one note, and in them the tone depends on the elasticity of the mouthpiece. The bronchi can be thought of as this trumpet, where the opposite walls are in contact and where the air current produces, when separated, a musical note. A large, squishy mass, when vibrated, will produce a low note (rhonchi), while the tone will be high (wheezing) when the oscillating tissue is light and hard (Figure 25-3).
Therefore, the tone of the "wheeze" is independent of the length of the bronchus. The vibrating tissue can be represented by stenosis, secretions, tumors, etc.
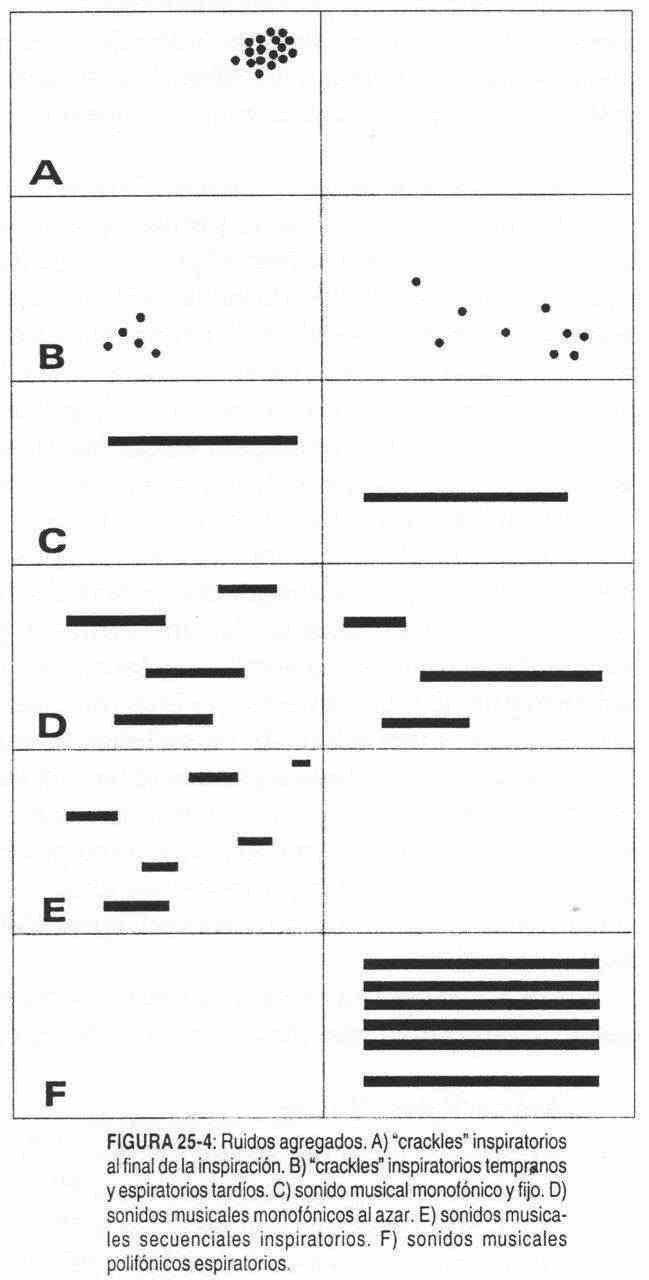
Continuous sounds can have a variety of musical components that, when they all begin and end at the same time, are called polyphonic (Figure 25–4, E). When musical components begin and end at different times (Figure 25-4, D) they are called monophonic.
The continuous sounds or "wheezes" are characteristic of obstructive pulmonary diseases.
Clinical applications
Monophonic and fixed continuous or "wheeze" sound . It is characteristic of incomplete occlusion of a main or lobar bronchus due to tumor, foreign body, cicatricial stenosis, or intrabronchial granuloma (Figure 25-4, C). If the mass that occludes the bronchial lumen is large, the tone of the "wheeze" will be low. They can be inspiratory or expiratory, or at both moments of respiration and can be modified with changes in the patient's position.
Random monophonic continuous sounds . Airways narrowed by mucosal spasm or edema can produce random musical sounds or monophonic "Wheezes" (Figure 25-4, D). They can be inspiratory or expiratory, or found in inspiration and expiration. Their amplitude is great and they are well transmitted to the wall. Those that originate in the central bronchi are heard at the level of the mouth and in the thoracic wall, while the "wheezes" that originate in the peripheral routes are not heard in the mouth. They are characteristic of asthma.
Inspiratory sequential "Wheezes" . They are characteristically auscultated at the lung bases in stenosing alveolitis, asbestosis, and other interstitiopathies. They are of different tone, originate in collapsed territories that open late on inspiration and do not overlap each other (Figure 25-4, E).
Polyphonic expiratory "wheezes." In chronic bronchitis, and with forced expiration, it is possible to hear "wheezes" with the ear (Figure 25-4, E). The characteristic fact is that all the components concur at the same time until they end together at the end of expiration. Its good transmission to the mouth and the wall and its low tone indicate its central origin. They are an important sign of diffuse bronchial obstruction when they do not occur only in forced expiration. Healthy subjects can, with forced expiration, cause "wheezes".
Stridor . It is characteristic of laryngeal spasm.
Its mechanism is similar to that of phonation. In stridor the vocal cords are brought together not only by the action of the laryngeal muscles but also by the existing edema. A stridor can also be heard in tracheal stenosis. It will be inspiratory if the affected trachea is the cervical portion.
Paradoxical absence of "wheezes" . Some patients with diffuse bronchial obstruction do not generate "wheezes". This occurs in patients with chronic obstructive pulmonary diseases who have too low an airflow to cause them. This absence of "wheezes" should not be confused with an improvement in the patient.
"Crackles" or interrupted sounds
Crackles are short, explosive, non-musical noises heard through the chest wall, or through the mouth, and are attributed to the presence of bubbling secretions in the airways. This explanation is undoubtedly correct when there are secretions in the bronchi. However, it is not explained why they are usually confined to inspiration and why they occur in diseases such as alveolar fibrosis, in which there are no secretions.
Crackles are more likely to be produced by an explosive change in gas pressure, rather than by sudden oscillations in distended tissues. When the pressure gradients in the airway are small, the opening of these airways is silent. On the other hand, when a large change in gas pressure occurs, explosive noises can be generated without any involvement of the lung tissue. It is possible, however, that the walls of some airways are in contact for a short time after opening and that they produce little oscillation by a vibrating reed mechanism when they are separated. These oscillations end in three milliseconds and cannot be heard by the ear. It has been suggested that sudden distension of the alveoli can generate explosive noises, similar to those produced by a sailboat when filled with air, or a paper bag inflated to its highest capacity. However, the elastic properties of these hard materials are not similar to lung elasticity, and sudden inflation of a distended lung to its maximum capacity does not produce "crackles".
Intrabronchial gas pressure or traction on the expanding lung can open closed airways. In localized or universal airway obstruction, the gas pressure may be sufficient to reopen slightly occluded airways. The pressure gradient drops, and then the airway closes again. The passing of each aerial bolus is accompanied by an explosive noise. The cycle is reproduced several times in the course of a single breath, generating a series of "crackles". The intensity of the "crackle" depends on the differential pressure and the size of both reservoirs, and the tone is determined by the resonance frequencies of the gaseous compartments and their solid limits.
In deflated lungs, such as fibrosing alveolitis, many peripheral airways remain closed until a late stage of inspiration. When the lung expands and elastic tension rises, these pathways open one by one and remain open for the remainder of inspiration. The opening of each airway is accompanied by a "crackle". In other words, "crackles" can be produced by the sequential opening of different airways or by the repeated opening of the same airway during the respiratory cycle. The "crackles" of the same sequence can be generated by any mechanism; spaced "crackles" of equal loudness indicate repeated opening of the same airway.
Crackles heard at the level of the anterior chest wall, in subjects who breathe low lung volumes, are not necessarily abnormal.
Clinical applications
"Crackles" at the end of inspiration . They are a characteristic sign of pulmonary fibrosis and interstitial pulmonary edema (Figure 25-4, A). They are also heard in poorly ventilated territories, such as when diaphragmatic movements are restricted, or in normal subjects during the first breaths after a shallow and prolonged breath.
Its distribution is basal and symmetric.
These "crackles" are heard profusely at the end of inspiration and are repeated with each respiratory cycle, and since they are poorly transmitted, they change with small movements of the stethoscope.
They are rarely heard in the mouth. Some "crackles" cease immediately with changes in position, others become more widely spaced, and others are unchanged. All these clinical conditions suggest that these "crackles" are a sign of delayed opening of the small airways.
In interstitial fibrosis, asbestosis, and other diffuse interstitial fibrosis, some alveoli are filled with cells or destroyed by fibrosis. Healthy alveoli receive greater air volume, and show little compliance due to these successive changes in respiratory volume.
In the resolution phase of lobar pneumonia, with alveoli filled with exudate, the alveolar respiratory excursion is extremely long. As in alveolar fibrosis, a pressure gradient is created, where the reopening of the alveoli is delayed until the end of inspiration.
In left ventricular failure and pulmonary hypertension they are attributed to the bubbling of pulmonary edema. The "crackles" in interstitial edema are due to an equalization of gas pressure that occurs at the end of inspiration when the alveoli narrowed by the peribronchial edema open.
Another important fact is the disappearance of "crackles" with changes in posture, which will serve to assess the degree of severity of the lung disorder. They will be more affected if they are not modified with changes in posture; if they do it in the horizontal position due to the force of gravity they will be less affected.
"Crackles" in early inspiration and late expiration . They are common in early airway obstruction, low-pitched, and rare and frequent (Figure 25-4, B). They are also transmitted to the large airways and therefore can be heard with the stethoscope in the patient's mouth.
These "crackles" originate due to the passage of gas through a slightly narrowed path, which opens intermittently when the gas reaches the critical pressure. Their scarcity, their good transmission and the fact that they are heard in the mouth, mean that their origin is in the central roads.
Whatever the mechanism of intermittent closure of the large bronchi, the correlation between these "crackles" and air obstruction is well established. These "crackles" correlate well with obstructions measured in the spirometer, while late "crackles" do well with restrictive diseases or in which the FEV (1) / CV (forced expiratory volume in the first second / vital capacity).
Inspiratory basal cracks . They are found in chronic bronchitis and left heart failure, and their differences are listed in Table 25-1. The difference with fibrosis is added, which can be an evolutionary sequence of both.
| Table 25-1 | ||
| Fibrosis | Chronic bronchitis | Left heart failure |
| Late | Early | Late |
| Scarce | Scarce | Profuse |
| Medium tone | Low tone | High tone |
| Not transmitted | Transmitted to the mouth | Inaudible in the mouth |
| They don't change with posture | They are not affected by posture | They are modified with the position |
Pleural rubs or "crackles" . Fibrin deposits in the pleural sheet (inflammatory or by neoplastic cells) produce changes in the resonance, causing a musical sound or a series of non-musical sounds. This pleural rub is characterized because the sounds heard in inspiration tend to be heard in expiration, giving a mirror image.
Pleural "crackles" of less than five milliseconds duration are indistinguishable from those of pulmonary origin. They increase with compression of the stethoscope.
"Crackles" in the pneumothorax . In the left pneumothorax, strong or high crackles can be heard along the left edge of the sternum and synchronized with the heartbeat. They are strongest at the end of expiration and when the patient is lying on the left side. These sounds originate in the pleural space, either by a sudden displacement of air trapped in the mediastinal pleura or by impact of the heart on the mediastinal aspect of the lung.
Loose cough . During coughing, noises similar to those heard in airway obstructions can be heard, giving the sensation of expectoration in the airways. Healthy subjects who cough voluntarily have loud noises, but no adventitious sounds.
The association of loose cough and diffuse bronchial disease is well documented and correlates well with: 1) smoking, 2) history of bronchitis, 3) daily sputum, 4) alterations in spirometry. The loose cough is related to rapid oscillations of the airflow during the expulsion of air, due to the collapse with rebound in the air walls, and corresponds to the intermittent passage of air in the obstructed airways.
Voice auscultation
Under normal conditions, the frequency of the formants is not well transmitted to the chest wall. When there is no air in the lungs, between the trachea and the auscultation point, that is, the normal parenchyma is altered, the vocal formants and high frequencies are transmitted correctly, and then the auscultated voice becomes understandable. This phenomenon is called bronchophonia, and it is found when the lung has consolidated and the bronchus remains patent.
When the separate vocal cords do not oscillate, as in the whispered voice, the sound is produced by turbulent oscillations in the trachea, pharynx, and glottis. Normally, this voice is not transmitted due to a lack of low tones. In the consolidated lung, on the other hand, it is perfectly auscultated. This phenomenon is called aphonic pectoriloquia; has the same physiological bases as bronchial respiration auscultated in the chest wall and bronchophony, and together with them constitutes the triad of consolidation
In pleural effusions and pneumothorax, the voice and breath sounds are inaudible. The condensation that may exist above a small layer of pleural effusion allows only the transmission of high frequency sounds (1000 Hz), giving the auscultated voice the characteristics of a nasal voice. This phenomenon is called egophony. The patient is asked to say the letter I and is listened to with the stethoscope on the chest wall at the level of condensation, the letter E.
Table 25-2 summarizes the basic semiological findings in the main pathological processes that affect or affect the lung.
|
Table 25-2 Pulmonary semiology in different pathological processes |
||||
| Percussion | Vocal vibrations | Auscultation | Added noise | |
| Congestive heart failure | Sound (when there is no spill) | Normal | Breathing sounds |
Inspiratory-expiratory "cracks" at the bases. |
| Pneumonia | Mate | Augmented |
Bronchophonia Egofonia Pectoriloquia aphona Bronchial sound |
Inspiratory-expiratory "Crackles" |
| Bronchitis | Sonorous | Normal | Prolonged expiration | "Wheezes" y "Crackles" |
| Emphysema | Hypersonoro | Diminished | Decreased breath sounds and prolonged breathing | |
| Pleural effusion | Mate | Decreased or absent |
Decreased or abolished respiratory sound Bronchial breathing and egophony |
Rub occasionally |
| Pneumothorax | Hypersonoro | Decreased or absent | Decreased or absent breath sounds | |
| Atelectasis with obstructed bronchus | Mate | Decreased or absent | Decreased or absent breath sounds | |
| Atelectasis without obstructed bronchus | Mate | Augmented |
Decreased or absent breathing sound Bronchial sound |
"Wheezes" y "Crackles" |
| Asthma | Sonorous | Diminished |
Expiration Breathing sound |
"Wheezes" at first in inspiration, then in both respiratory times |