by Alberto J. Muniagurria and Eduardo Baravalle
The examination of the extremities includes evaluation of the skin and tañeras, adipose tissue, muscle masses, vascular system (venous and arterial), and nervous, osteoarticular, and lymph node systems. Usually begins with the examination of the nails and hands.
Nail
Nails should be thoroughly inspected for changes in color, shape and consistency, size, and the presence of furrows, spots, and inflammatory lesions. The nail bed is a very useful site to evaluate the concentration of hemoglobin, as much or more than the conjunctiva. Cyanosis can also be seen clearly.
The onicólisis , or destruction of the nails, is in fungal infections, hyperthyroidism and psoriasis. In the latter case, a desquamative condition of the skin, they acquire the shape of thimble nails (Figure 31-1), with a dotting; they are also seen in alopecia areata.
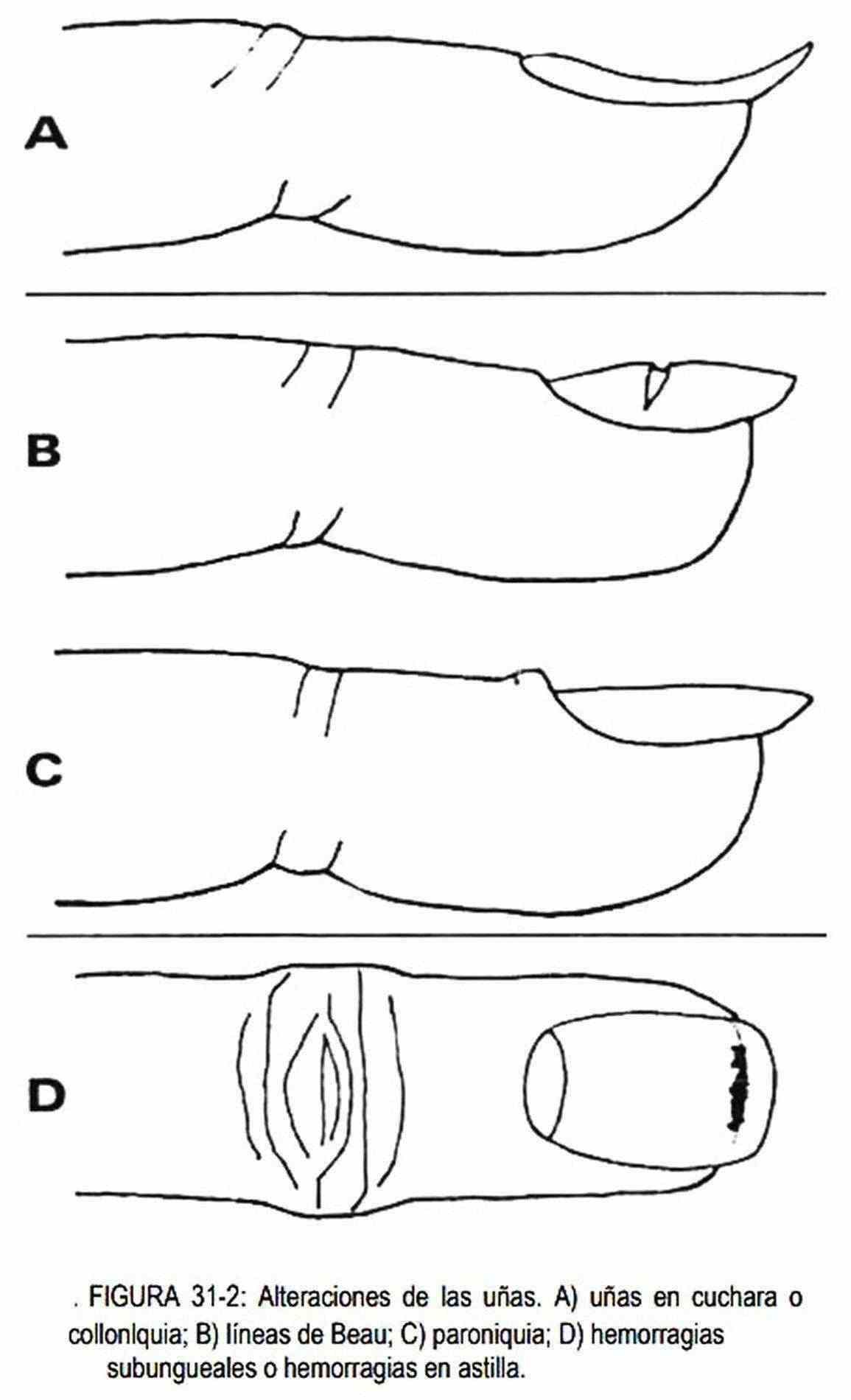
The spoon nails, or koilonychia (Figure 31-2, A), are deformed longitudinally concave. They can be seen in iron deficiency anemias, coronary heart disease, and systemic disorders such as syphilis, acromegaly, and hypothyroidism, and by the use of strong soaps; they can also be of family origin.
The fotoonicólisis is the destruction of the nail by exposure to light. This phenomenon occurs in some patients who ingest tetracyclines. In onychogryposis, or hypertrophy of the nails, the nail becomes a true claw; It is generally seen on the first toe in the elderly and careless patients, and in syphilis, neuritis, leprosy, hemiplegia, and repeated trauma. Onychauxis is the thickening of the nail plate and occurs due to trauma, circulatory insufficiency, syphilis, leprosy, and is rarely congenital. Pachyonychia is a thickening of the entire nail, more solid and regular than onychogryposis; It is usually of congenital origin or may be associated with hyperkeratosis of the palms and soles.
The Beau 's lines (Figure 31-2, B) are transverse lines or linear depressions arising level lunula and advancing progressively as the nail grows. They occur in situations of stress or great catabolism (infections, heart attack, childbirth, toxic syndrome) and result from a temporary arrest of the growth of the nail. Since nails grow 0.1 mm per day, by measuring the distance between the cuticle and Beau's line, the approximate date of trauma can be calculated.
The lines Terry are transverse white lines with red tips that can be observed in patients with liver cirrhosis, but also in normal individuals. In leukonychia, the nails are wholly or partially white, and the disorder may be seen in some cirrhotic or nutritionally deficient patients.
The lines Mee are white transverse bands seen in poisoning from thallium and arsenic, nutritional disorders, high fever and Hodgkin's disease.
The lines Lindsay, nails or half and half , are characterized by the proximal half white and half the distal reddish. They are found in kidney failure.
The aniquia is inflammation of the nail matrix with deformation of the nail bed.
The onychodystrophy is the deformity of the matrix, or nail plate bed, while called onicoatrofia to atrophy or failure in developing nails, trauma, infection, gonadal aplasia, etc.
The subungual hemorrhages or splinter hemorrhages (Figure 31-2, D) will be observed as longitudinal lines, reddish, in the nail bed, accompanying bacterial endocarditis, trichinosis and vasculitis; they also appear without apparent cause.
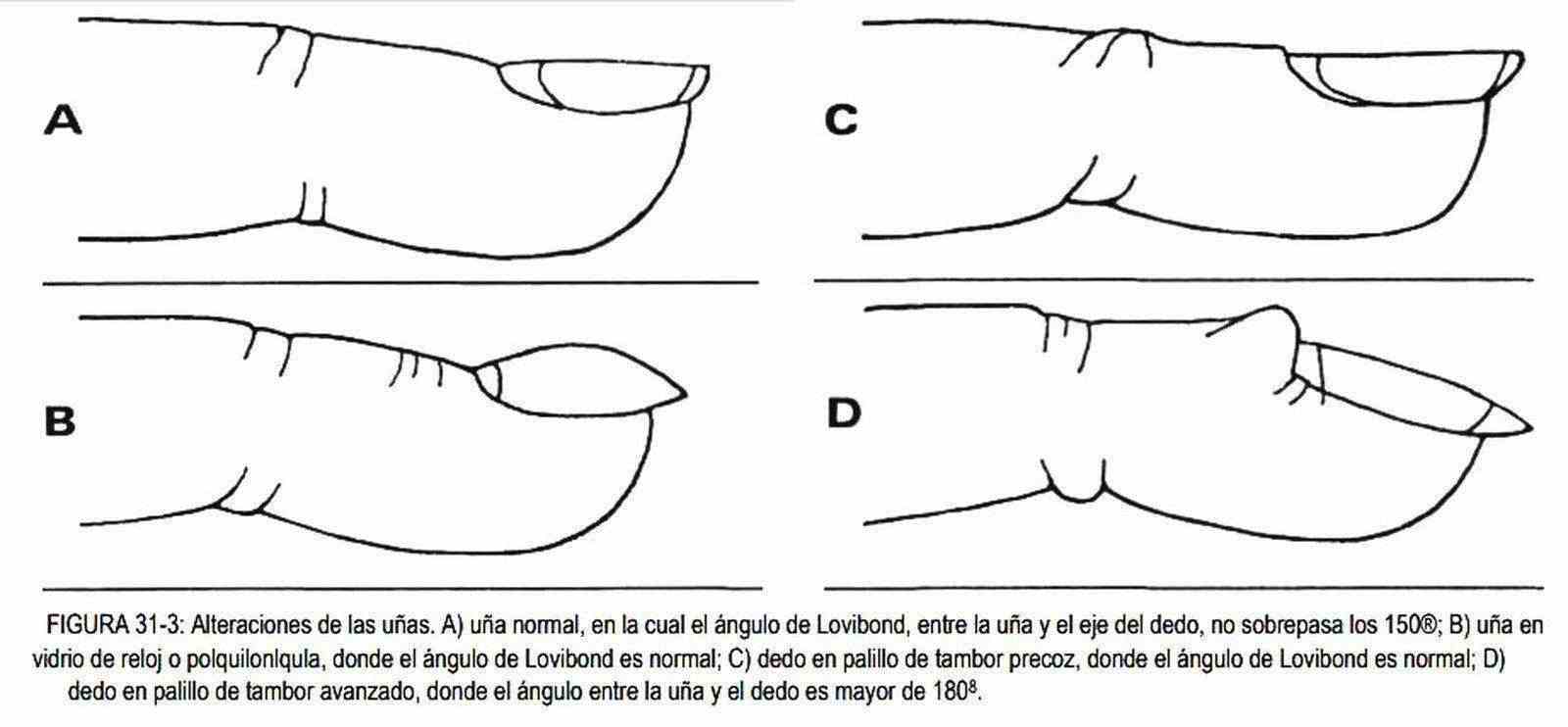
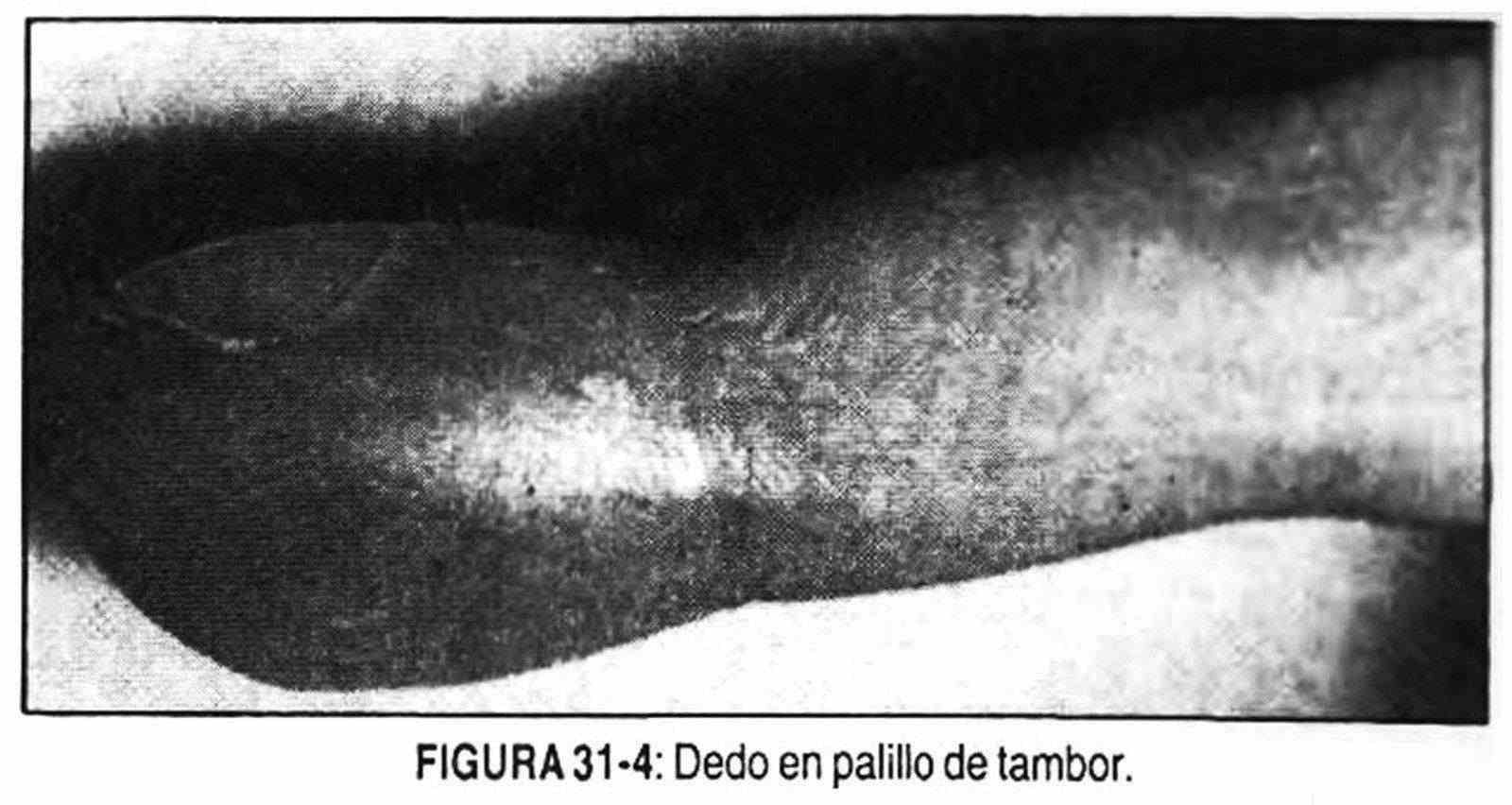
the poiquiloniquia, or watch glass nails (Figure 31-3, B), is the exaggerated convexity of the nails. This is a normal variant in which the angle between the base and the nail has been preserved, a fact that the difference of the drumstick finger, or "clubbing" (Figure 31-3, C v D and Figure 31-4 ). This angle formed between the base of the nail and the nail is called the Lovibond angle and under normal conditions it should not exceed 160 °. Clubbing, or drumstick fingers, is a soft tissue edema with fibroelastic proliferation and minimal mononuclear infiltration, resulting in a bun at the end of the fingers. The Lovibond angle exceeds 180 °. The etiology of "clubbing" is uncertain, although it is probably related to blood flow through multiple arteriovenous communications in the distal phalanges. This disorder can develop with or without pneumatic hypertrophying osteopathy and may be accompanied by watch glass nails.
The onychomadesis is the complete loss of nails and is seen in diseases such as syphilis, leprosy, exfoliative dermatitis and scarlet fever. In hapalonychia the nails are fragile due to having been in contact with strong alkalis or due to malnutrition, syphilis or cyanotic diseases.
The extent of the lunula occurs in the extremities dystrophies. The so-called eggshell nails are transparent and bluish-white, with a tendency to convexity. They are seen in nutritional deficiencies, syphilis, or trauma. Brittle nails that break easily are usually due to dietary deficiencies.
The paronychia (Figure 31-2, C) is swelling and inflammation with pain of the skin around the nail. It is also called perionixis. Onyxis is the inflammatory lesion of the nail and is usually accompanied by perionixis. If the infection takes the base of the nail, a subungual abscess can form. Chronic inflammation of the periungual ridge is seen frequently in mycoses, psoriasis, and diabetes. Monilia (Candida albicas) nail infection occurs frequently in dishwashers, gardeners, and dentists.
The nail biting is a habit of biting his nails, and onicotilomanía is the alteration produced by persistent pulling nails. The presence of longitudinal fissures with division of the nails is called onychorrhexis, and it is observed in skin or infectious diseases, in hyperthyroidism, senility and due to the action of chemical agents. These same causes can lead to onychoschisis, which is the peeling of the nails in layers.
The unguis pterygium consists of the thinning of the nail fold with growth of the cuticle on the nail plate. It is observed in Raynaud's phenomenon.
Superior members
Alterations in the shape and size of the hands. In acromegaly, a disease of tumor origin caused by abnormal secretion of somatotrophic hormone by pituitary cells, large hands with sausage fingers are observed, along with other alterations caused by the exaggerated growth of cartilage.
In Hurler's disease or gargoylism the hand is thick-skinned and the shape and size are modified by widening and shortening of the long bones. The hands can also become deformed and enlarged in Maffucci syndrome, which is caused by enchondromatosis of the long bones and cavernous hemangiomas in the soft tissues. In this syndrome, it is possible to observe one hand larger than the other, a fact that is also seen in arteriovenous fistulas and aneurysms.
In certain cases, such as Paget's disease, the hands are irregularly enlarged, and can be painful and deformed. Multiple exostoses is another inherited bone dystrophy where the metacarpals are shortened with numerous exostoses. The trident hand is a short hand with stubby fingers that is seen in achondroplasia.
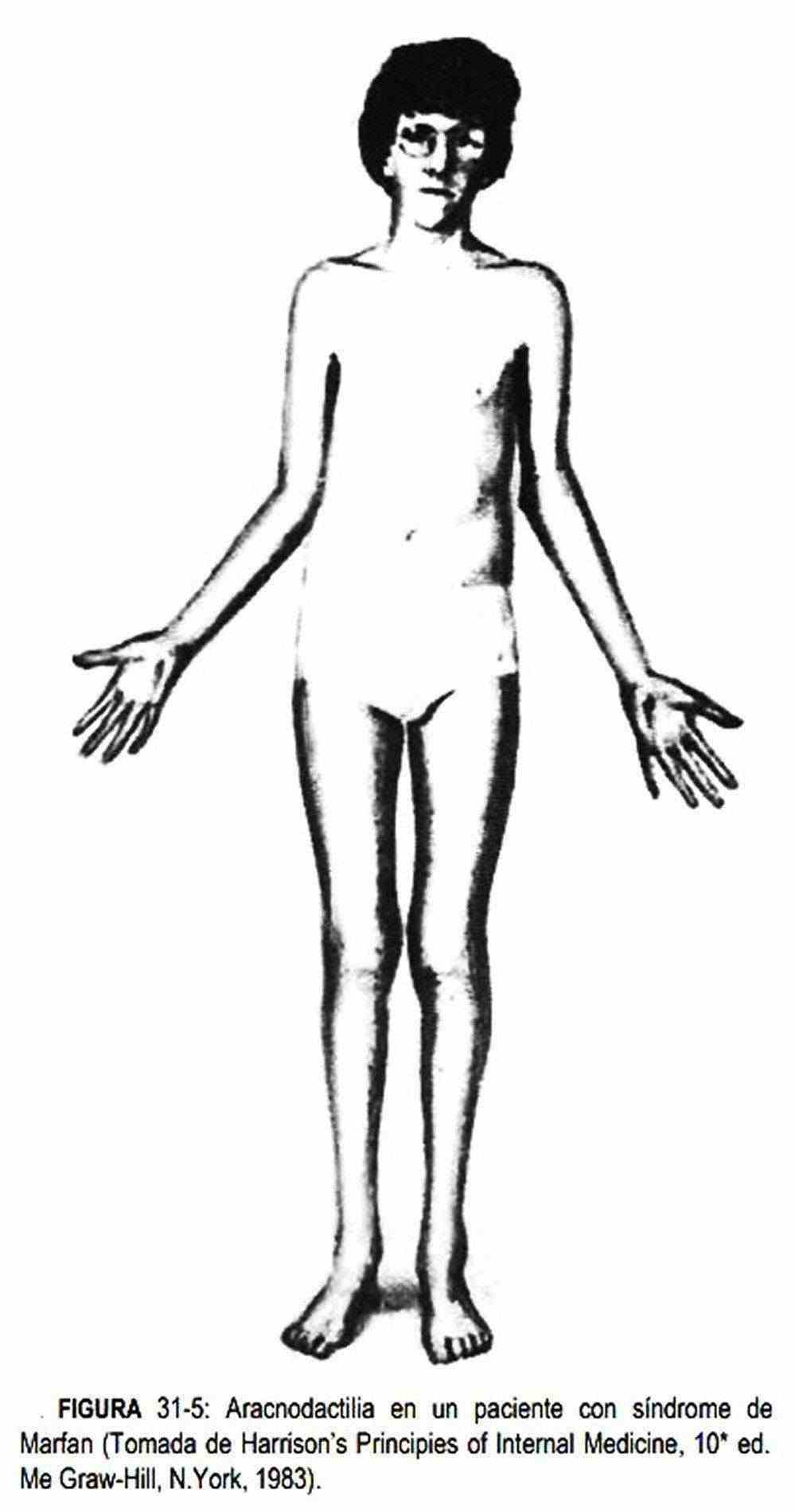 Sometimes the hands have long, thin fingers, with a sharp appearance and an elongated palm, as seen in arachnodactyly or spider fingers.
Sometimes the hands have long, thin fingers, with a sharp appearance and an elongated palm, as seen in arachnodactyly or spider fingers.
Radiographically, the metacarpal index can be calculated, which consists of dividing the length of the last four metacarpals by their width and averaging the results. In normal individuals this index is less than eight; an index above eight is suggestive of Marfan syndrome. Arachnodactyly (Figure 31-5) is seen in Marfan syndrome, hypopituitarism, tuberculosis, osteogenesis imperfecta, Ehlers-Danlos syndrome, and asthenic individuals. Sharp fingers are described in osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus, and rubella, psoriasis, and sarcoidosis.
Cone-shaped fingers, in turn, are seen in pituitary obesity and Frohlich syndrome.
In cretinism or congenital hypothyroidism, and in addition to a number of other manifestations, the hands are square and the skin is dry.
Shortening of the metacarpals, also called brachymetacarpalism, when it occurs in the fourth and fifth fingers should suggest pseudo- and pseudo-hypoparathyroidism. When the fifth finger occurs and it is bent, it is called Dubois symptom, observed in Mongolism and Gargoylism; poor position with abduction of the fifth finger is described in Turner syndrome.
There are also other congenital disorders that affect the shape and size of the hand. Syndactyly is the presence of an interdigital membrane; It is usually accompanied by other congenital alterations, such as vascular and cardiac, and is seen in hereditary form and in Lawrence Moon-Biedl syndrome.
Polydactyly is the presence of supernumerary fingers. Ectrodactyly is the lack of one or more fingers, while brachydactyly is the decrease in normal length. There is acromelia or phocomelia when the hands and / or feet are born directly from the trunk.
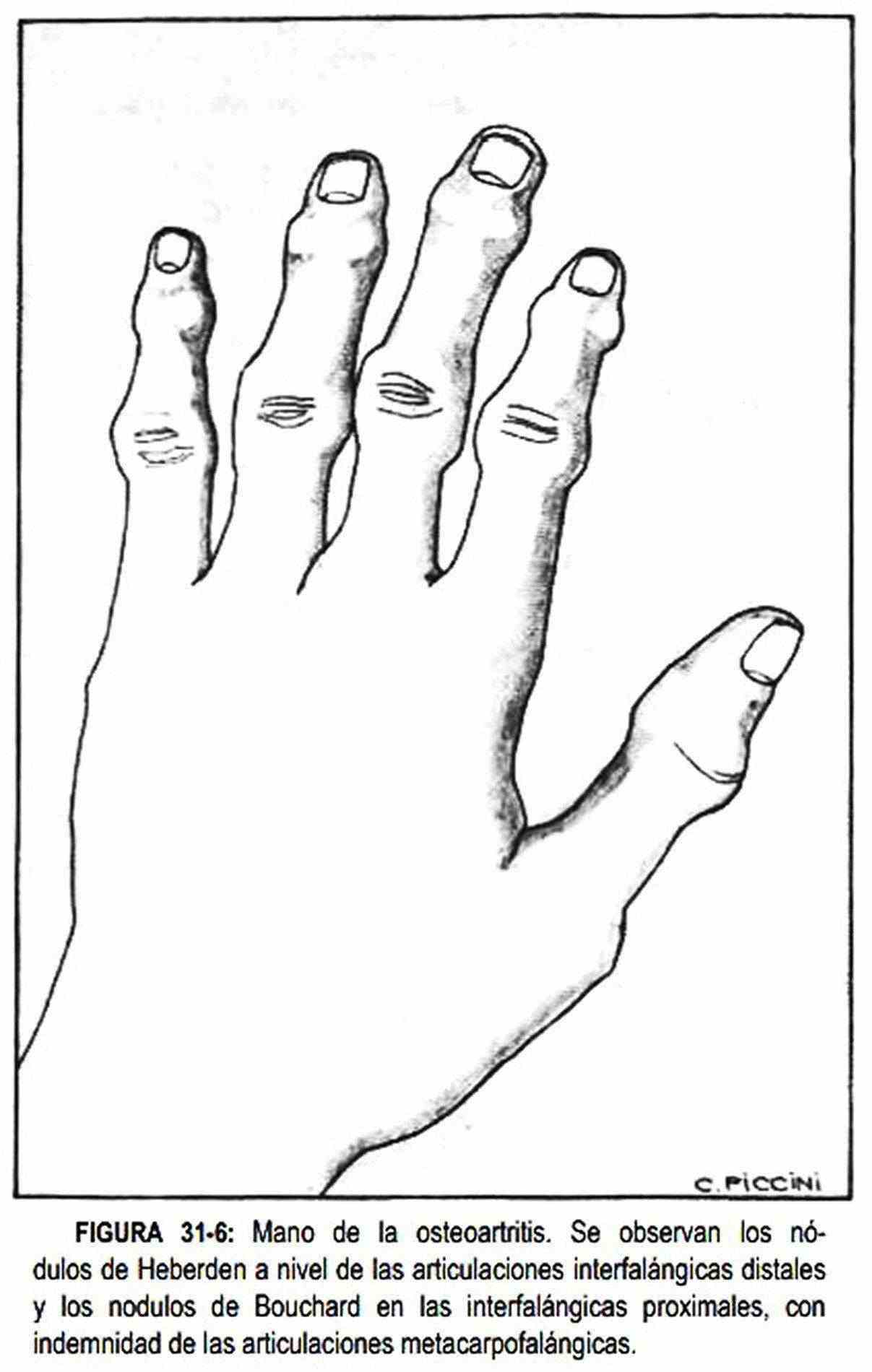
Sometimes the shape of the hands is altered by joint diseases. In osteoarthritis or osteoarthritis (Figure 31–6), nodules are seen in the distal interphalangeal joints, called Heberden's nodules; when they occur in the proximal interphalangeals, they are called Bouchard's nodules.
They characteristically do not affect the metacarpophalangeal joints and are hard, painless nodules.
They are accompanied by radial deviation of the distal phalanges.
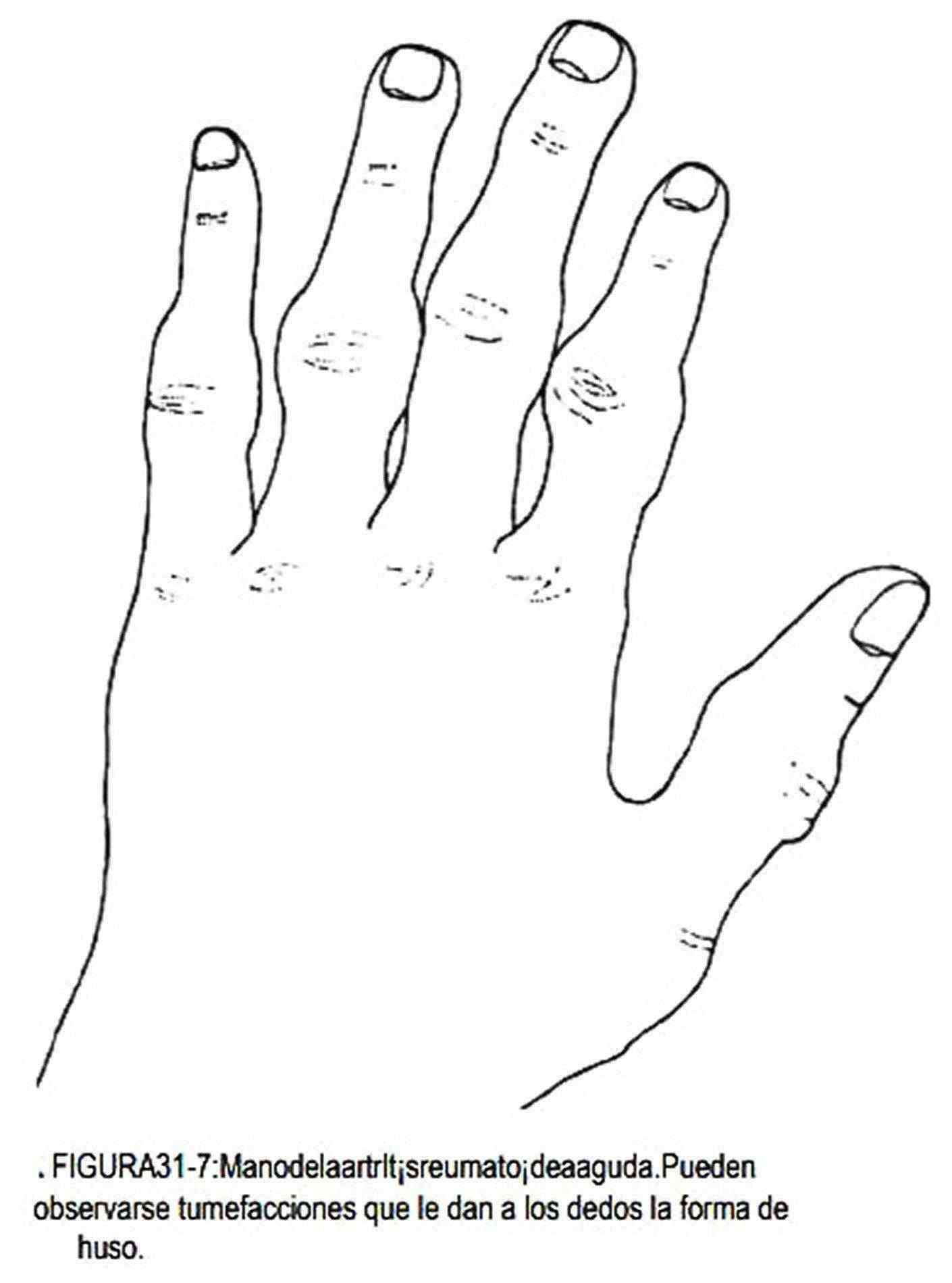
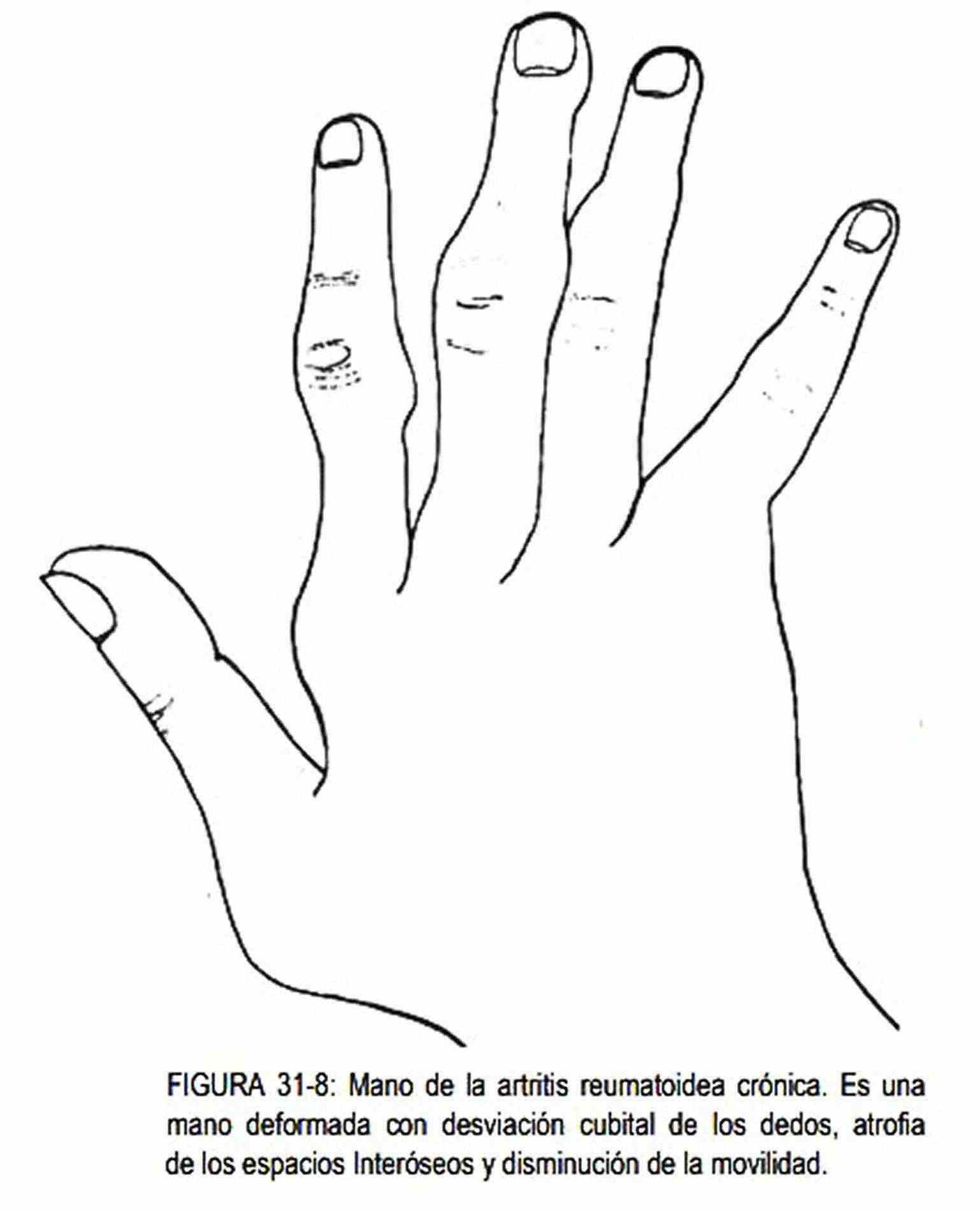
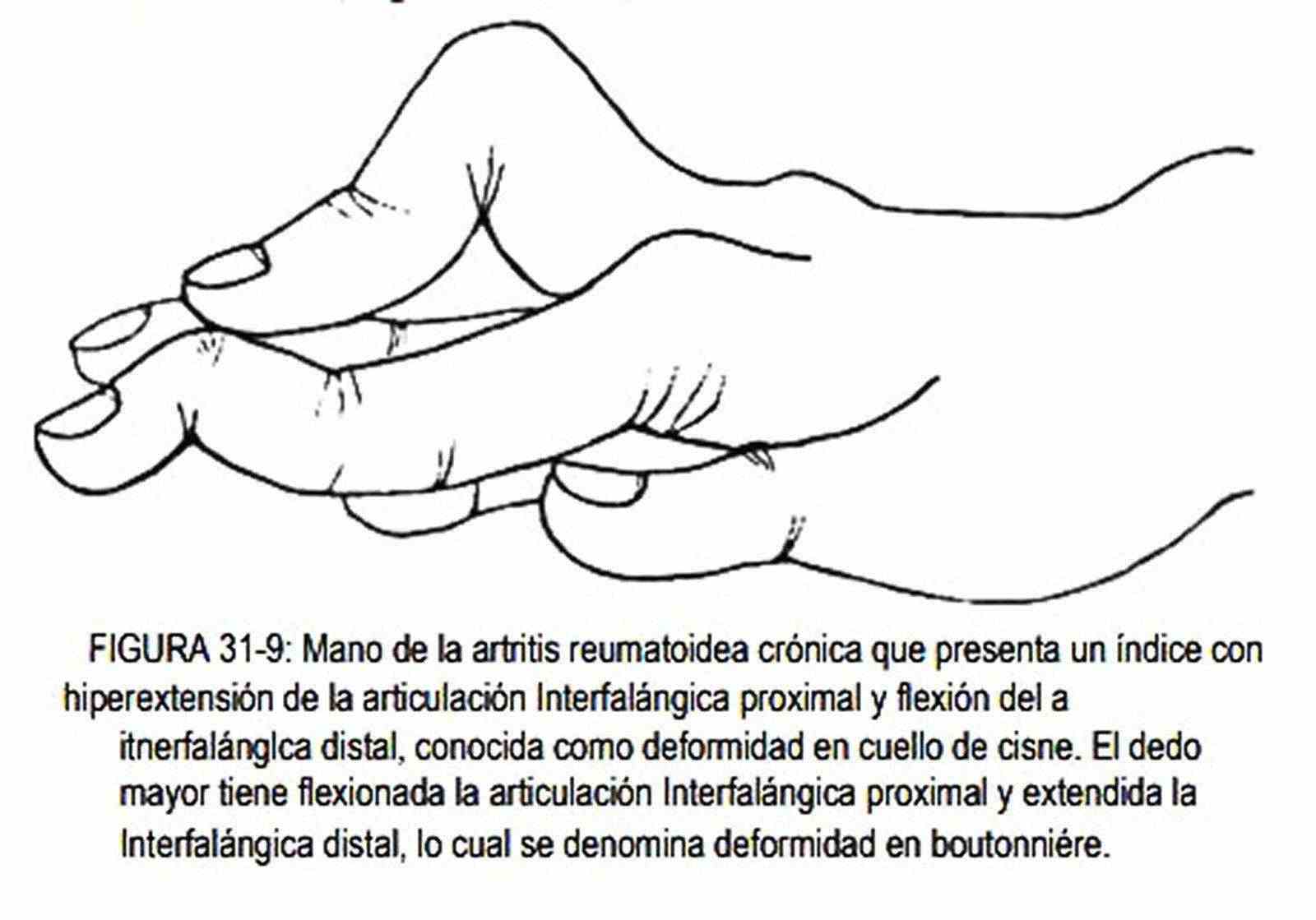
The hand may be painful and tender, with stiff joints, as occurs in the acute phase of rheumatoid arthritis. This disease is characterized by being bilateral and symmetric, and frequently affects the proximal interphalangeal or metacarpophalangeal joints and the wrist. The distal interphalangeal joints are usually spared, a fact that does not occur in psoriatic arthritis. The hand appears spindle-shaped or spindle-shaped (Figure 31-7). In the chronic phases, with chronic edema and widening of the metacarpophalangeal and proximal interphalangeal joints, movements are limited. The fingers deviate to the ulnar side (Figure 31-8), and the interosseous spaces atrophy. When there is hyperextension of the proximal interphalangeal joint with fixed flexion of the distal interphalangeal joint, the swan neck finger is produced (Figure 31-9). Less common is finding persistent flexion of the proximal interphalangeal joint with hyperextension of the distal interphalangeal joint, constituting the "boutonniere" deformity (Figure 31-9).
It is also possible to observe nodules in the extensor tendons, called rheumatoid nodules, which are one of the diagnostic criteria for this disease. In rheumatic fever, nodules can also appear, painless, from millimeters to two centimeters, firm, mobile, located on bony prominences or tendons.
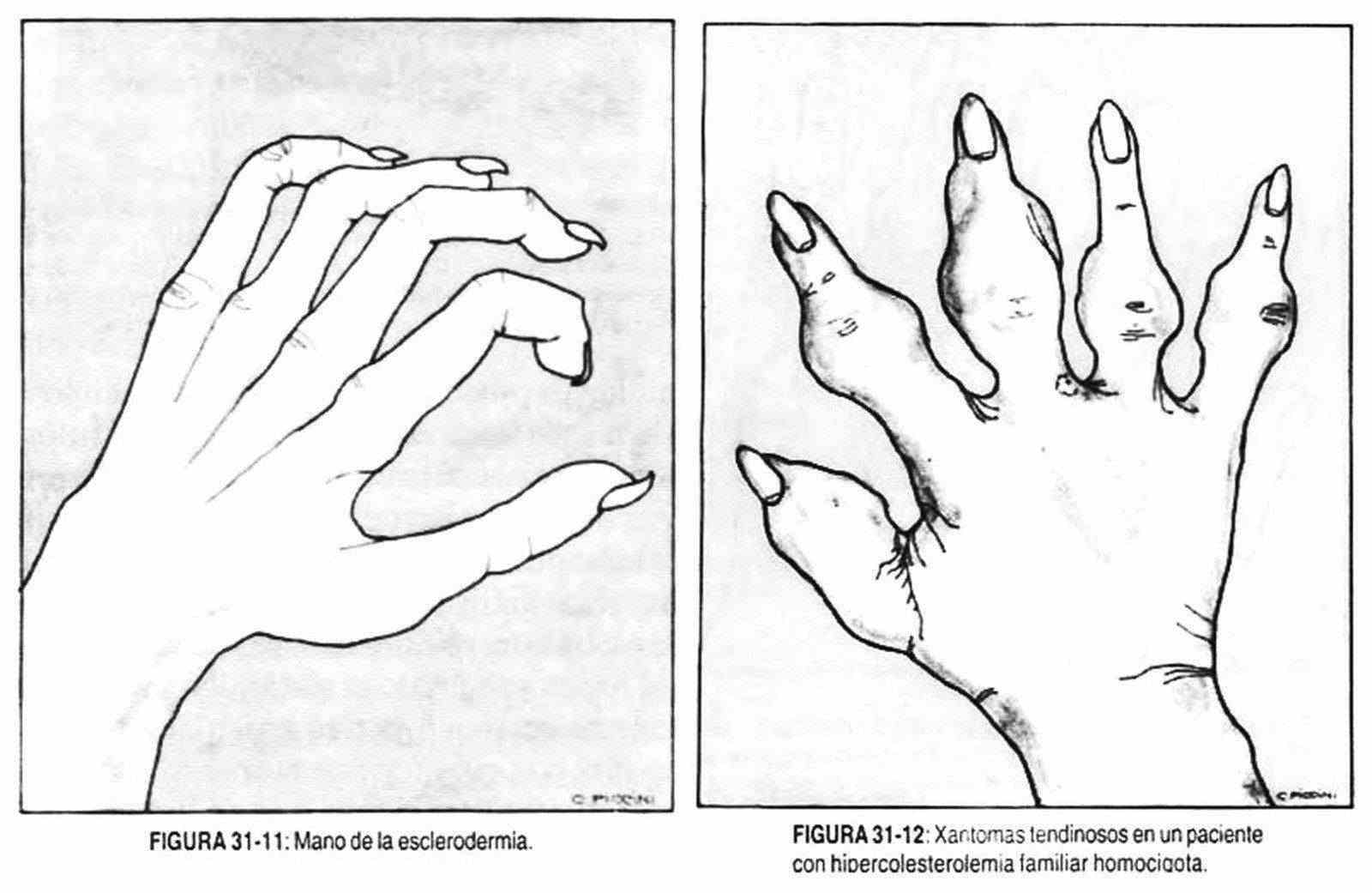
In systemic lupus erythematosus, edema can be observed in one or more joints of the hand, with redness and a local increase in temperature, alterations that are not generally symmetrical, as in rheumatic fever; in this last entity they have the particularity of being migratory. In gout (Figure 31-10), the hand has characteristics similar to those of osteoarthritis and rheumatoid arthritis. The acute phenomenon need not be present and uric acid crystal deposits or tophi are seen in the joints. These tophi can secrete a chalky material, sometimes even ulcerating. There are also joint manifestations in dermatomyositis, Reiter's syndrome, and sarcoidosis.
At other times, the shape is altered by the presence of a pneumatic hypertrophying osteopathy, which consists of a periostitis in which the periosteum is lifted by a new bone matrix with endostal bone reabsorption. It occurs in the hands and feet and in the distal part of the long bones, wrists, and ankles. With disease progression, these changes can affect the clavicles, scapulae, and ribs. There is pain, synovial thickening with chronic swelling and edema, and proliferation of fibroblasts in the joint capsule. All these phenomena produce fattening of the fingers. It is seen in intrathoracic neoplasms and previously it was seen in pulmonary suppurations; In general, it can be said that the same causes that produce "clubbing" or clubbing of the fingers can cause hypertrophying pneumonic osteopathy, and this may or may not precede or follow clubbing. The intimate mechanism of its production is not known, but it is associated with the presence of arteriovenous communications and neurogenic and / or humoral mechanisms, and it may or may not be accompanied by watch glass nails. Drumstick fingers can be seen in some lung diseases (lung or pleural neoplasms, bronchiectasis, empyema, pneumoconiosis, interstitial fibrosis); in cardiovascular diseases (congenital heart disease, subacute bacterial endocarditis, in advanced pulmonary heart, pulmonary arteriovenous fistula); in diseases of the digestive system (sprue, ulcerative colitis, regional enteritis, alcoholism, biliary cirrhosis, liver abscesses, amyloidosis); in poisonings (arsenic, phosphorus and beryllium); in hyperthyroidism (coexisting with telescoping of the distal phalanx), hyperparathyroidism, chronic pyelonephritis, syringomyelia, chronic granulocytic leukemia, polycythemia, and myxedema, and may also be familial.
Likewise, "clubbing" can be asymmetric, as occurs in median nerve injuries or when there is an innominate artery aneurysm or recurrent shoulder subluxation.
Hammer toes, or baseball players, are caused by the rupture of the extensor tendon on the third phalanx due to a sudden flexion of the finger in extension. Spring or trigger fingers cannot be flexed, and with increasing effort, movement occurs abruptly; the extreme degree is called blockage. It is due to flexor tenosynovitis or buttonhole rupture of the extensor aponeurosis. The wide and flattened phalangeta is seen in sarcoidosis, and the cone-shaped fingers, as discussed earlier, can be seen in Frohlich's dystrophy and in pituitary obesity.
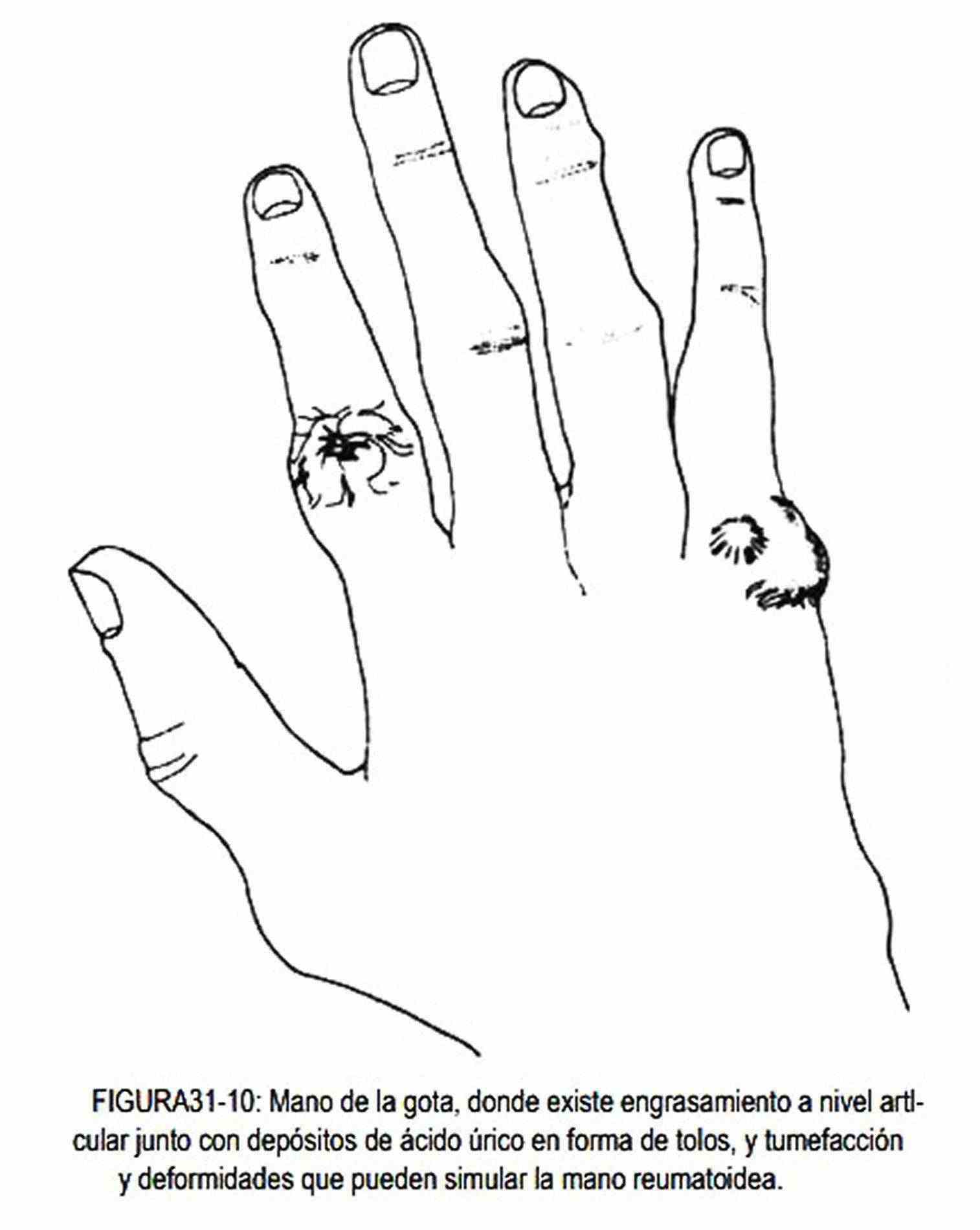
Scleroderma (Figure 31-11) causes retraction of the skin with marked bone and joint reliefs. The skin is stretched, there is limited mobility, and skin ulcerations can coexist.
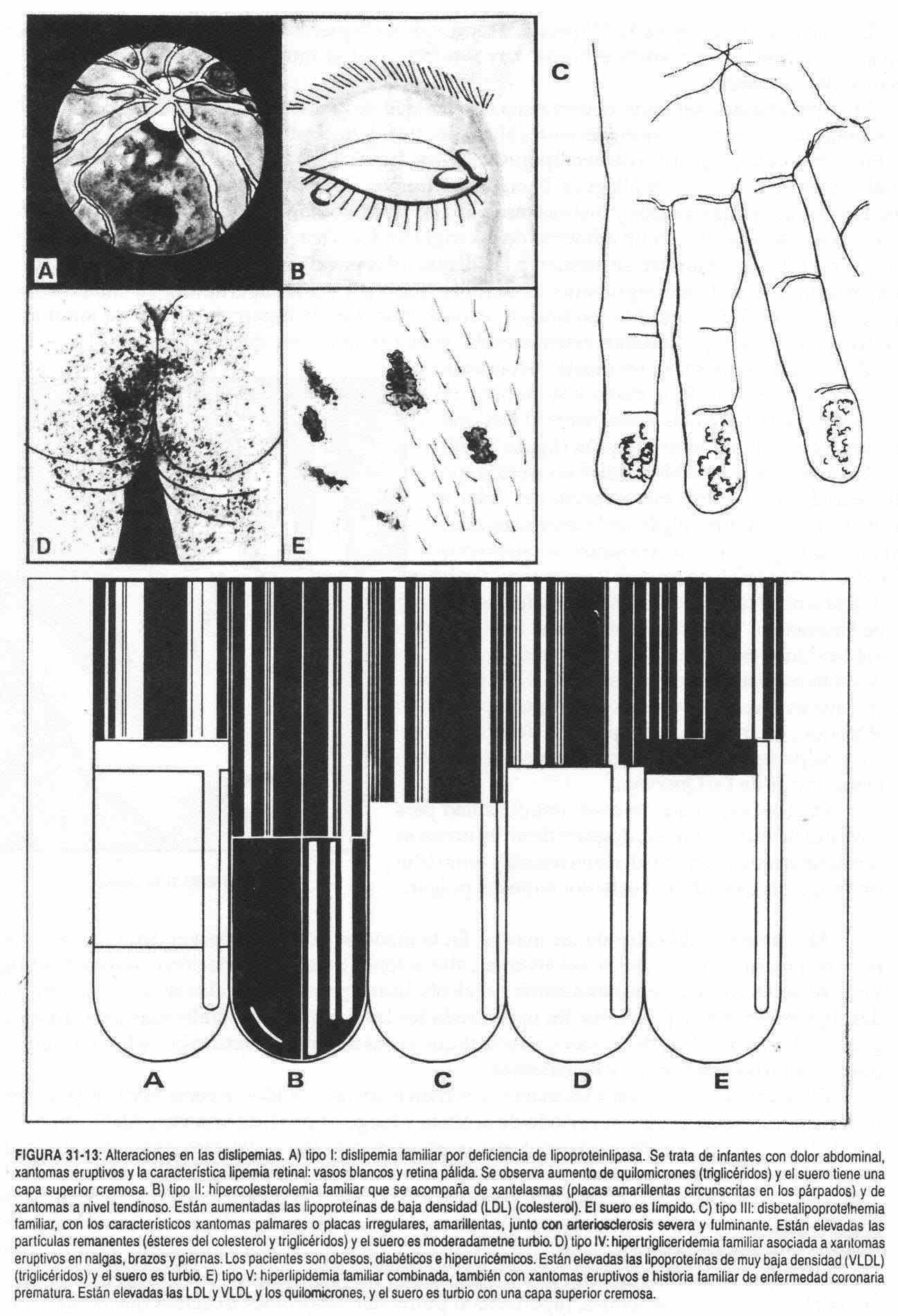
In certain hyperlipidemias, a deformity of the hand is observed due to the deposition of cholesterol in the tendons, which occurs in patients with familial hypercholesterolemia (Figure 31-12). In type III dyslipidemia or familial dysbetalipoproteinemia, yellowish plaques are seen on the palms of the hands, fingers, and folds, called xanthomas. Eruptive xanthomas have a predilection for the buttocks, arms, and legs; are yellow-orange papules located on an erythematous base and are associated with increased triglycerides or familial hypertriglyceridemia (type IV), but are also associated with dyslipidemia due to familial lipoprotein lipase deficiency (type I), familial dysbetalipoproteinemia (type IV) III) and familial combined hyperlipidemia (type V). Tendon xanthomas,
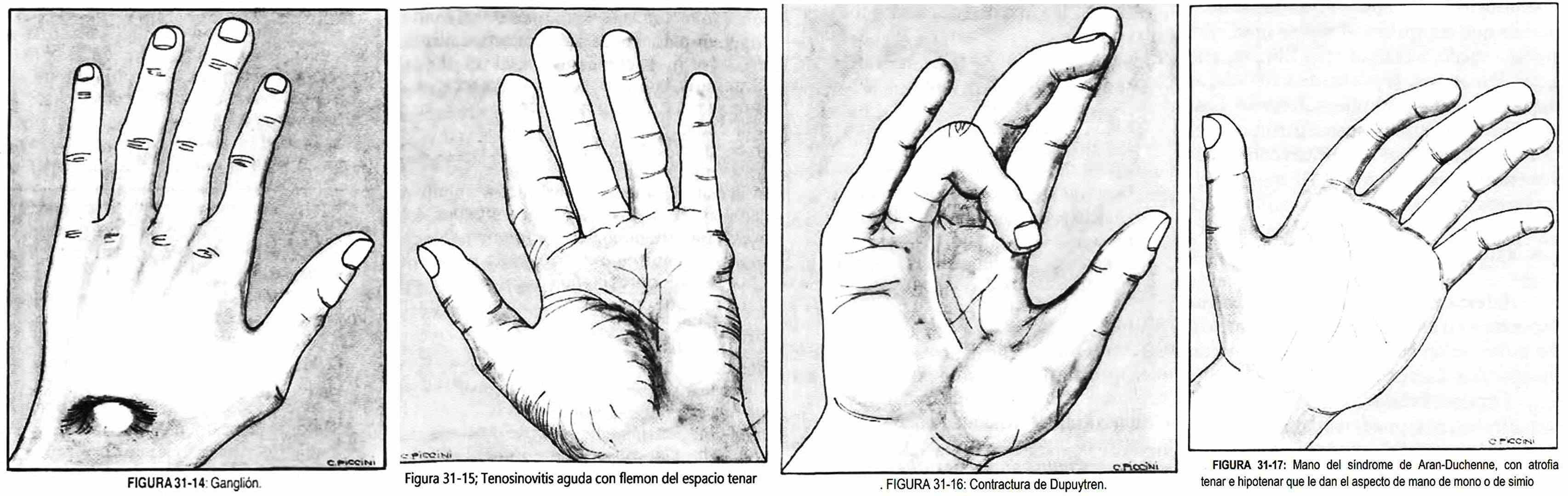
Other times, a non-painful, rounded cyst is seen on the extension side of the hand and wrist, which becomes more prominent when the hand is flexed. This is the so-called ganglion (Figure 31-14).
The presence of a painful nodule on the radial styloid process, with exacerbation of pain when passively flexing the thumb with the wrist in ulnar adduction, is typical of stenosing tenosynovitis of the abductor pollicis longus and the extensor pollicis brevis at the level of the process Styloid radius (Finkelstein's sign). The disorder is due to the continuous rubbing of the tendon on the sheath during various tasks, in washerwomen, pianists, athletes, etc. Evolutionarily, the tendon sheath thickens and compresses the tendon, determining the appearance of the visible and palpable nodule; The condition is known as De Quervain's tenosynovitis.
On other occasions, there is difficulty in mobilizing the thumb, which, after an effort, is achieved abruptly (spring finger), as occurs in tenosynovitis of the extensor pollicis longus.
Alterations in the color of the hands . Color changes can be observed in the hand, such as cyanosis, paleness in anemias, pigmentation changes such as vitiligo, and redness in dermatomyositis and alcoholism; yellow palms in carotinemias; and depigmentation and purples. Sometimes generalized purples produce blue folds in the palm of the hand, while petechiae and bruises may appear in different hemorrhagic diseases.
Sometimes the fingers and hands turn white and pale, sometimes from exposure to cold; subsequently there is a period of acalmia and then there is vasodilation with flushing.
The disorder is more frequent in women, in the hands, which, in the feet, is symmetrical and can lead to the production of ulcers. This is the so-called Raynaud's phenomenon, which is observed in chronic arterial diseases, collagen diseases (scleroderma, eosinophilic fasciitis, mixed connective tissue disease, systemic lupus erythematosus, dermatomyositis, CREST syndrome), industrial or occupational diseases (as in workers using vibrating objects), due to the use of medications such as ergotamine or propanolol, in hematological diseases, dysproteinemia, pulmonary hypertension, thoracic syndromes that obstruct the arteries that go to the upper limb (for example: supernumerary ribs), occult carcinomas, and exposure to toxins such as lead and arsenic.
The tips of the fingers and toes may present diffuse cyanosis, with coldness and perspiration; It is the so-called acrocyanosis, which is not accompanied by any underlying disease. Livedo reticularis is a benign disorder characterized by a persistent cyanosis, mottled in appearance with a network appearance, which is not confined exclusively to the fingers, but may involve the extremities and trunk. It is accentuated with exposure to cold.
 Chilbladder or erythema pernio is observed in children and young people, in autumn and winter, and appears as red-bluish, itchy spots, especially on the hands and feet. It can have other locations in territories poorly defended from the cold, and is caused by vasculitis induced by exposure to cold. Cold injury or immersion injury, which affects any age and gender, occurs in both the hands and feet. The member is pale, cyanotic, and cold, and can occasionally become gangrenous.
Chilbladder or erythema pernio is observed in children and young people, in autumn and winter, and appears as red-bluish, itchy spots, especially on the hands and feet. It can have other locations in territories poorly defended from the cold, and is caused by vasculitis induced by exposure to cold. Cold injury or immersion injury, which affects any age and gender, occurs in both the hands and feet. The member is pale, cyanotic, and cold, and can occasionally become gangrenous.
In causalgia, which is a sympathetic dystrophy that affects people under 50 years of age, patients consult for pain that appears before mechanical stimuli or cold, both in the upper or lower limbs and in other locations, with a sudden onset and long duration.
The limb is cyanotic, painful, and swollen. Pulsatile discoloration changes at the fingertips, or Quincke pulses, are described in aortic regurgitation, hyperthyroidism, anemia, and high fever.
On the back of the hand, hyperpigmentation of the veins has been observed in Hodgkin's disease. Other times there is diffuse melanosis on the back or in the lines of the palm of the hand associated with Addison's disease. In argyrosis, a grayish pigmentation can be seen. In manual workers, a yellowish palmar hyperkeratosis may be observed, especially at the points of support.
Alterations in the temperature of the hands . The temperature of the hand may increase in fever, hyperthyroidism, erythromelalgia, and arteriovenous fistulas, and in joint or bone diseases (Paget's disease). Conversely, it can be reduced in all states of hypoperfusion, whether of general origin such as shock, or peripheral, such as cold or arterial occlusion. It is also decreased in collagen diseases, acrocyanosis, Raynaud's disease, and by administration of drugs, such as beta blockers.
Patients with erythromelalgia, both men and women, generally under sixty years of age, complain of pain, burning and itching with exertion or with exposure to cold or heat, usually in the feet and legs, less commonly in the hands; the condition is sudden onset and is accompanied by swelling and heat during the attack, together with an increase in temperature and a reddish coloration of the skin. This syndrome may be primary or accompany polycythemia vera, arterial hypertension, systemic lupus erythematosus, myeloproliferative disorders, and treatment with bromocriptine.
Localized swellings in the hand . Hand edema can be seen in heart, liver and kidney diseases and in patients with hemiplegia, syringomyelia, superior vena cava syndrome, hypoproteinemia with anasarca, postmastectomy lymphedema, ischemic paralysis, axillary lymphatic obstruction due to tumors, leukemias, Hodgkin's disease , compression on the subclavian vessels, Raynaud's disease, myositis, supernumerary rib, trichinosis, scalene syndrome.
Localized swelling of the fingers and palms is also seen in acute infectious processes. Infection of the flexor tendon sheath may follow minor or trivial local injury. The pain and edema are located along the tendon - and not in the joints - from the distal phalanx to the metacarpophalangeal joints. The finger is held in slight flexion as an analgesic position. If the infection progresses, it can reach the palmar fasciae and cause swelling in the thenar and hypothenar eminences or in the middle palmar space. These pictures can be initiated by manipulations of a manicure on the nails and by periungual processes.
The whitlow is the pyogenic infection of the fingers at the level of the cell spaces, the tendon sheath, the joint cavity and the bone cell, and is more frequent in the thumb and index finger. Chancre-like lesions are occasionally seen in actinomycosis, tuberculosis, anthrax, syphilis, leishmaniasis, sporotrichosis, and tularemia.
Phlegmons have different locations according to the tendon distribution of the hand, and can be commissural, middle palmar, or the thenar and hypothenar spaces (Figure 31-15).
Injuries to the palms . On occasions, progressive hypertrophy of the palmar aponeurosis is observed with retraction of the flexor tendons of the fingers of the hand. Initially, indurated skin nodules appear at the root of the ring finger, with retraction in flexion of the ring finger on the palm and the impossibility of extension. It usually affects the ring finger and follows in order of frequency, the little finger and the middle finger. The disorder is seen in normal middle-aged people or in alcoholics, diabetics, patients with Raynaud's disease, scalene syndrome, syringomyelia, or after a myocardial infarction. This is called Dupuytren's contracture (Figure 31-16).
 It is also possible to find palmar xanthomas, which are observed as small nodules with irregular contour and are located on the extensors of the hand; they are associated with familial hypercholesterolemia, and diabetes, nephrotic syndrome, Gaucher disease, Niemann-Pick and von Kierke diseases, and in myxedema.
It is also possible to find palmar xanthomas, which are observed as small nodules with irregular contour and are located on the extensors of the hand; they are associated with familial hypercholesterolemia, and diabetes, nephrotic syndrome, Gaucher disease, Niemann-Pick and von Kierke diseases, and in myxedema.
In the palm, the so-called palmar erythema can be observed, more visible in the thenar eminence, which can appear in healthy people, in cirrhotic patients, ("hepatic palm"), in alcoholics, polycythemics, in diabetes, in vitamin B1 deficiencies, in hyperestrogenism and collagen diseases, and it is also described in mitral regurgitation.
Mucocutaneous erythematous ganglionic syndrome, or Kawasaki disease, is characterized by a maculoerythenate eruption on the hands and feet and is accompanied by fever, rhinitis, and gingivitis, and later by cervical lymphadenopathy, pyuria, proteinuria, and diarrhea. It is seen in children and adults; it is occasionally associated with meningitis.
Painful, erythematous, or purpuric nodules may appear on the palmar aspect of the fingers, the palms of the hands, or the soles of the feet, probably representing embolic lesions of bacterial endocarditis and are called Osler's nodules. Other times, non-painful erythematous maculopapular subcutaneous lesions, called Janeway spots, are observed, also associated with bacterial endocarditis.
In Mongolism there is a single transverse fold in the palm of the hand.
Hand alterations caused by neuromuscular diseases . Neuromuscular diseases can produce some hands with particular characteristics.
- Hand of median nerve palsy. Also known as the monkey hand, it presents atrophy of the thenar eminence, with a predominance of the adductor pollicis.
- Hand of radial palsy. It is a pendulous hand, due to paralysis of the extensors of the fingers. If it is also accompanied by paralysis of the carpal extensors, the wrist will be flexed.
- Hand of ulnar palsy. Also called claw hand, it is characterized by atrophy of the small muscles of the hand and hyperextension of the fingers at the level of the metacarpophalangeal joints, with flexion of the interphalangeal joints. It is also known as the ulnar claw.
- Preacher's hand. It is a hand with forced extension due to atrophy of the flexors of the forearm and of the small muscles of the hand. It is seen in sirignomyelia. When the skin is smooth, shiny and cold, cyanotic in color and edematous in appearance due to hypertrophy of the subcutaneous and bone tissue induced by sirignomyelia, it takes the name of succulent hand.
- Hand of Wilson's disease (or hepatolecticular degeneration). In this hand the last three fingers are flexed, with the thumb and index finger in a parkinsonian attitude (flexed and joined).
- Thalamic hand. In this case the fingers are hyperextended in a dystonic attitude, with tremor.
- Parkinsonian hand. The hand is pronated, flexed, over the thoracoabdominal region, with a static tremor especially of the thumb and forefinger, and in an attitude of counting coins.
- Zamba hand. Congenital or acquired, the hand folds over the forearm, ending in a rounded extremity.
- Skeletal or scleroderma hand. It has already been described separately.
- Aran-Duchenne syndrome hand. It is characterized by progressive evolution and begins with atrophy of the thenar and hypothenar eminence muscles, giving it the appearance of a monkey or ape hand (Figure 31-17). Later atrophy of the extensor muscles of the first phalanx and of the flexors of the second and third phalanx appears. Generalized atrophy of the hand results in a skeletal hand. This atrophy can be unilateral or bilateral. When bilateral, it is generally due to degenerative processes of peripheral motor neurons, the classic example being amyotrophic lateral sclerosis; It can also be caused by any process, intra or extramedullary, that damages the cervical thickening. When it occurs unilaterally, it can be caused by traumatic injuries to the palm of the hand,
- Hand on horn. It is due to the atrophy of the common common muscle of the fingers, without compromise of the extensor of the index and little fingers, and can be observed in lead poisoning.
- Midwife hand. The fingers are squeezed into a cone shape, as in the position of the midwife's hand when it enters the uterus. It is characteristic of hypocalcemia, whatever its etiology, and constitutes the so-called Trousseau sign.
- Contracted hand in flexion. In this case the nails can penetrate the palm, and it is also known as the fakir hand; it can be seen in syringomyelia, leprosy, and hemiplegia.
In patients with sensitivity alterations and dermal spots, the epitrocean area should be palpated in search of lymphadenopathy and / or thickening of the ulnar nerve, characteristic disorders of leprosy.
Tremors . They can be thin or thick and persist or not during rest. They are observed in Parkinson's disease, in the so-called essential or senile family tremor, hypoglycemia, hyperthyroidism, Wilson's disease or hepatolenticular degeneration, anxiety, ataxia, athetosis, alcoholism, drug addiction, amyotrophic lateral sclerosis , chorea, certain cerebellar lesions, hepatic coma, paresis, cold, fatigue, red nucleus lesions, and barbiturate and heavy metal toxicity.
 Pain in the upper limb . The presence of pain in the upper limb should suggest numerous causes. That is why the questioning and the presence of associated signs and symptoms will be extremely useful.
Pain in the upper limb . The presence of pain in the upper limb should suggest numerous causes. That is why the questioning and the presence of associated signs and symptoms will be extremely useful.
The pain can be burning or burning in distal areas, as in causalgia (where it is accompanied by cyanosis and swelling with cold and dampness) or as in neuritis that accompany diabetes, alcoholism, vitamin deficiencies, porphyrias , lead poisoning, collagen diseases, etc.
On other occasions, pain in the wrist and hand, with paresthesias that are accentuated when the wrist is percussed and the carpus is compressed, is typical of carpal tunnel syndrome. The pain is more intense at night and sometimes the patient refers it to the arm. Evolutionarily, it can lead to atrophy of the thenar eminence, with dry skin on the thumb, index and middle fingers and decreased nerve conduction. It can be idiopathic due to tenosynovitis of unknown cause that compresses the median nerve between the carpal bones and the anterior annular carpal ligament, or caused by fibrosis, edema, trauma, tuberculosis and other granulomatous diseases, amyloid deposit, acromegaly, myxedema, pregnancy and deposit diseases (Hand-Schüller-Christian, Gaucher, Niemann-Pick).
In cervical radiculitis and osteoarthritis, pain and tingling may appear in the upper limbs, which increase with the mobilization of the neck. Also the pain in the upper limbs that increases with the mobilization of the shoulders may be due to the compression of the nerve paths by a thoracic rib, constituting the thoracic outlet syndromes.
Sometimes a painful picture may appear at the level of the wrist, caused by aseptic necrosis of the lunate and known by the name of Kienboeck's disease.
Edema and pain in the elbow . At the elbow, swelling and pain can be observed spontaneously or after trauma or when palpating the olecranon. It is the so-called olecranon bursitis.
Synovial inflammation and fluid accumulation are best perceived between the olecranon and the epicondyles. Arthritis of the elbow is accompanied by a tender, painful swelling.
Another possibility is to find subcutaneous nodules, painless, easily detachable from the skin, firm, which may or may not be fixed to the periosteum: they are rheumatic nodules. Painless nodules may also appear on the extensor face of the forearm, which sometimes ulcerate and secrete a chalky-like material. They are gouty tophi produced by accumulation of uric acid.
Pain in the epicondyle, where the extensor muscles of the forearm originate, is common in tennis players, due to the forced and repeated pronation-supination of the forearm; in these cases, the dorsiflexion of the wrist against resistance causes a characteristic pain in the epicondyle (Cozen test). In drug addicts it is possible to observe multipuncture zones, together with the existence of sclerosed and hyperpigmented venous cords with areas of hemorrhagic suffusion in different evolutionary stages. Foreign body lymphadenopathy or granulomas are common.
Pain in the shoulder. Acute pain in the shoulder, which increases during movement, especially in abduction and external rotation, occurs in inflammation with calcium deposits of the supraspinatus tendon. Inflammation progressively penetrates into the subacromial bursa, giving rise to bursitis. When calcium deposits are found in the tendons of the shoulder rotator muscles, the pain is chronic, beginning with the abduction of the arm until it is released at around 120 °. If the pain is maximum over the head of the humerus, at the level of the biceps tendon, any contraction maneuver of this muscle will produce pain in this area. It is due to tenosynovitis of the biceps. The pain-inducing maneuver consists of flexing the shoulder to 90 ° and asking the patient to try to supinate his arm against the resistance of the physician. A pain located just below the acromion along the humeral tube, with inability to abduct the arm after trauma, is due to the rupture of the supraspinatus tendon.
Fractures and other hand injuries . Hand fractures present with pain, after trauma. They are usually closed and can be spiral or transversal.
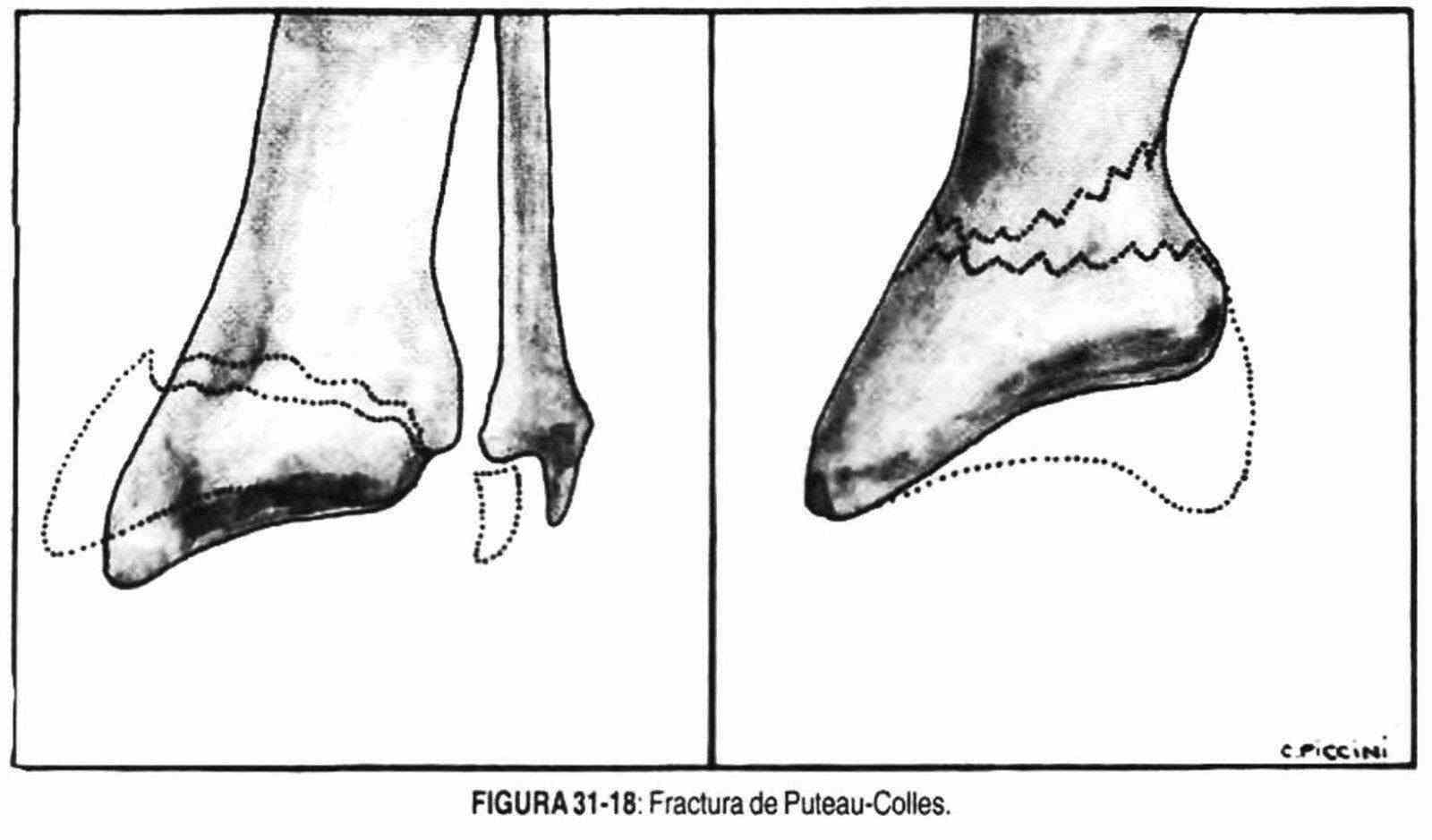
Palm-supported fall trauma can lead to edema and an extra-articular fracture dorsum deformity known as the Puteau-Colles fracture (Figure 31-18). It is a fracture of the lower extremity of the forearm, 15 mm from the wrist without reaching it, where the radial styloid is at the same height as the ulnar styloid. The most common finger dislocation is that of the dorsally displaced interphalangeal joints.
 Lower limbs
Lower limbs
 Alterations in the shape of the foot . Clubfoot does not rest on normal footholds, and it can be of congenital or acquired origin (poliomyelitis). There are various forms of clubfoot. In the clubfoot, the gait is carried out on the forelimb, with the heel away from the ground, while in the talus foot the foot rests exclusively on the heel. When it rests on the outer edge it is called the varus foot and when it does so on the inner edge it constitutes the valgus foot, with the sole directed outwards. Clubfoot frequently exhibits two of these deformities.
Alterations in the shape of the foot . Clubfoot does not rest on normal footholds, and it can be of congenital or acquired origin (poliomyelitis). There are various forms of clubfoot. In the clubfoot, the gait is carried out on the forelimb, with the heel away from the ground, while in the talus foot the foot rests exclusively on the heel. When it rests on the outer edge it is called the varus foot and when it does so on the inner edge it constitutes the valgus foot, with the sole directed outwards. Clubfoot frequently exhibits two of these deformities.
The flat foot is due to the relaxation of the plantar arch by abnormal elongation of the ligaments; the normal plantar arch has been lost.
In the pes cavus there is an imbalance of the long plantar muscles and the plantar aponeurosis, for which the foot is hollowed out and takes on the appearance of a stork leg.
In Friedrich disease (familial ataxia) the foot is in the varoequine position, with the sole well excavated, while the thumb is with the first phalanx in dorsal flexion and the second in ventral flexion, in Charcot-Marie dystrophy -Tooth muscle atrophy affects the peroneal muscles, and the interossei and extensor pollicis may also be atrophied.
The foot is shaped like a varoequino or pes cavus.
If voluntary dorsiflexion of the foot cannot be carried out and the patient is unable to walk with the heel, there is a paralysis of the external sciatic-popliteus, a frequent finding in women who wear high boots.
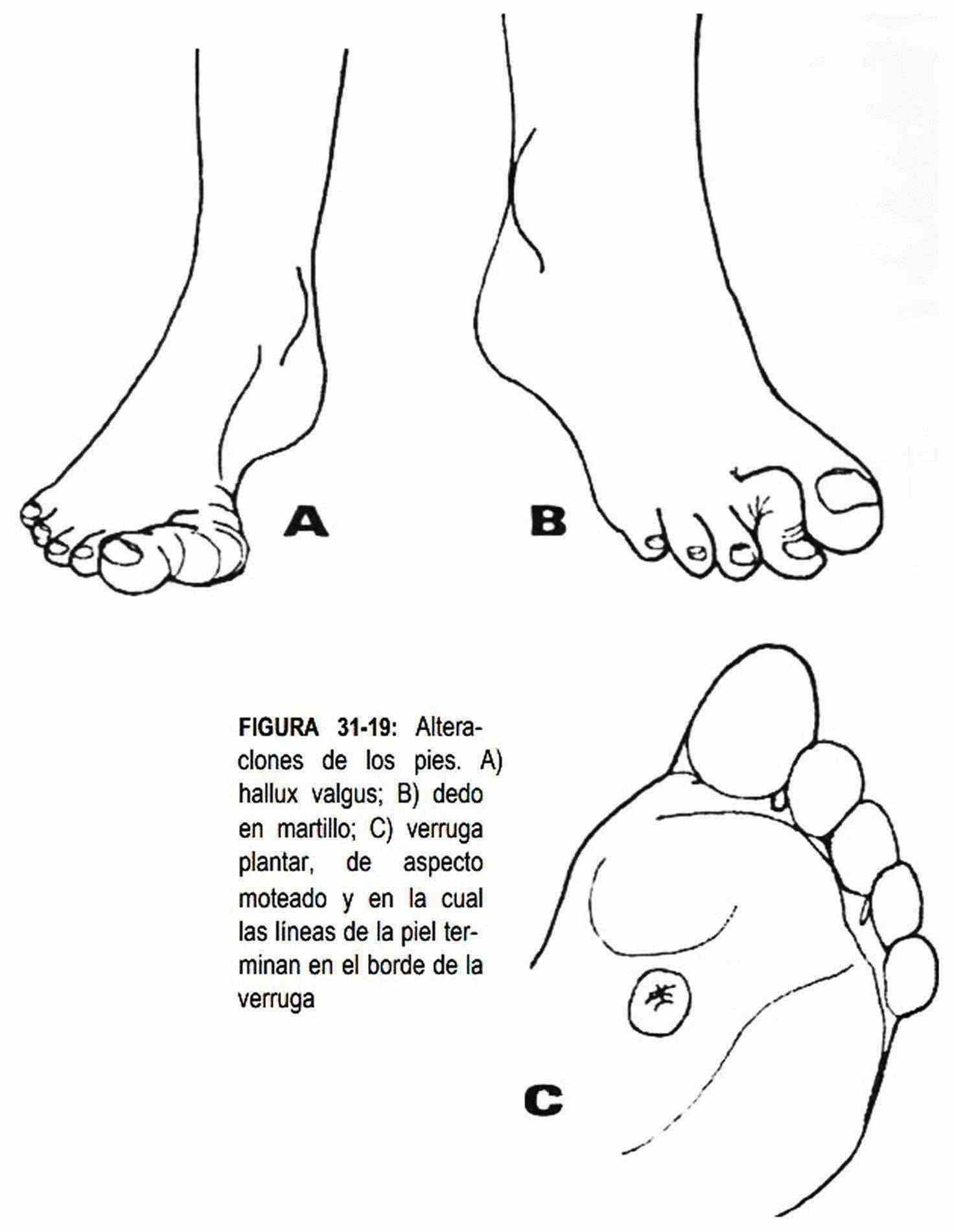
The foot can also be deformed by the presence of acute and chronic osteoarticular inflammatory processes, such as rheumatoid arthritis, osteoarthritis, gout, which have already been described. The metatarsophalangeal joint of the thumb is frequently affected in the attack of acute gout (podagra). The pain is intense, rubbing against the sheet makes it intolerable and the joint is red, hot and swollen. In the disease known as hallux valgus (bunion), this same joint is deformed, with the first toe turned outward and the first metatarsal turned inward (Figure 31-19, A). A painful bursitis may develop at the level of the first metatarsal head due to repeated pressure.
The edge of the nail on the first toe can penetrate and injure the skin fold, causing pain and infection. In this case, the fold is reddened and sometimes with purulent secretions. It is the so-called ingrown toenail .
When the metatarsophalangeal joint of one finger, the second usually presents hyperextension with flexion of the proximal interphalangeal, it is referred to as hammer toe (Figure 31-19, B).
The fifth finger can be found above or below the fourth finger, this malformation being called the fifth finger, supraduct or infraduct, respectively.
Osteoarticular alterations in the lower limbs . The foot and leg, due to their location, are frequently affected by trauma. Before a forced and sudden flexion of the foot, the tendon of the thin plantaris can rupture, with intense pain at the calf level. Other times the Achilles tendon ruptures, causing pain and inability to walk on the tip of the foot, along with the presence of swelling at the calf level due to retraction of the muscle.
The serous bursa that separates the Achilles tendon from the posterior aspect of the ankle can become inflamed and cause pain, swelling, limited movement, and crepitation at this level, characteristic of bursitis or tenosynovitis.
 The loss of sensitivity in the different neuropathies (syphilis, diabetes, syringomyelia, meningocele) exposes the joints to repeated trauma and can transform them into the so-called Charcot joints, which are observed deformed and destroyed, enlarged, with functional impotence and pain .
The loss of sensitivity in the different neuropathies (syphilis, diabetes, syringomyelia, meningocele) exposes the joints to repeated trauma and can transform them into the so-called Charcot joints, which are observed deformed and destroyed, enlarged, with functional impotence and pain .
As in the upper limbs, the joints can be affected by monoarticular or polyarticular processes.
These pictures are characterized by the presence of pain, redness, heat and joint swelling, as well as difficulty in active and / or passive mobilization. They can be of acute, subacute or chronic evolution, produce deformities and be accompanied by other alterations at the systemic level. This is how it is possible to find, when palpating the joint interline, thickening or signs of inflammation of the synovial membrane that orders the tendon sheaths. The diagnosis will be made from the evaluation of each of these variables.
Certain injuries to the hip cause functional impotence together with shortening of the affected limb and external rotation of the latter. Pain may be added to palpation of the groin region. These findings are characteristic of a fracture of the neck of the femur.
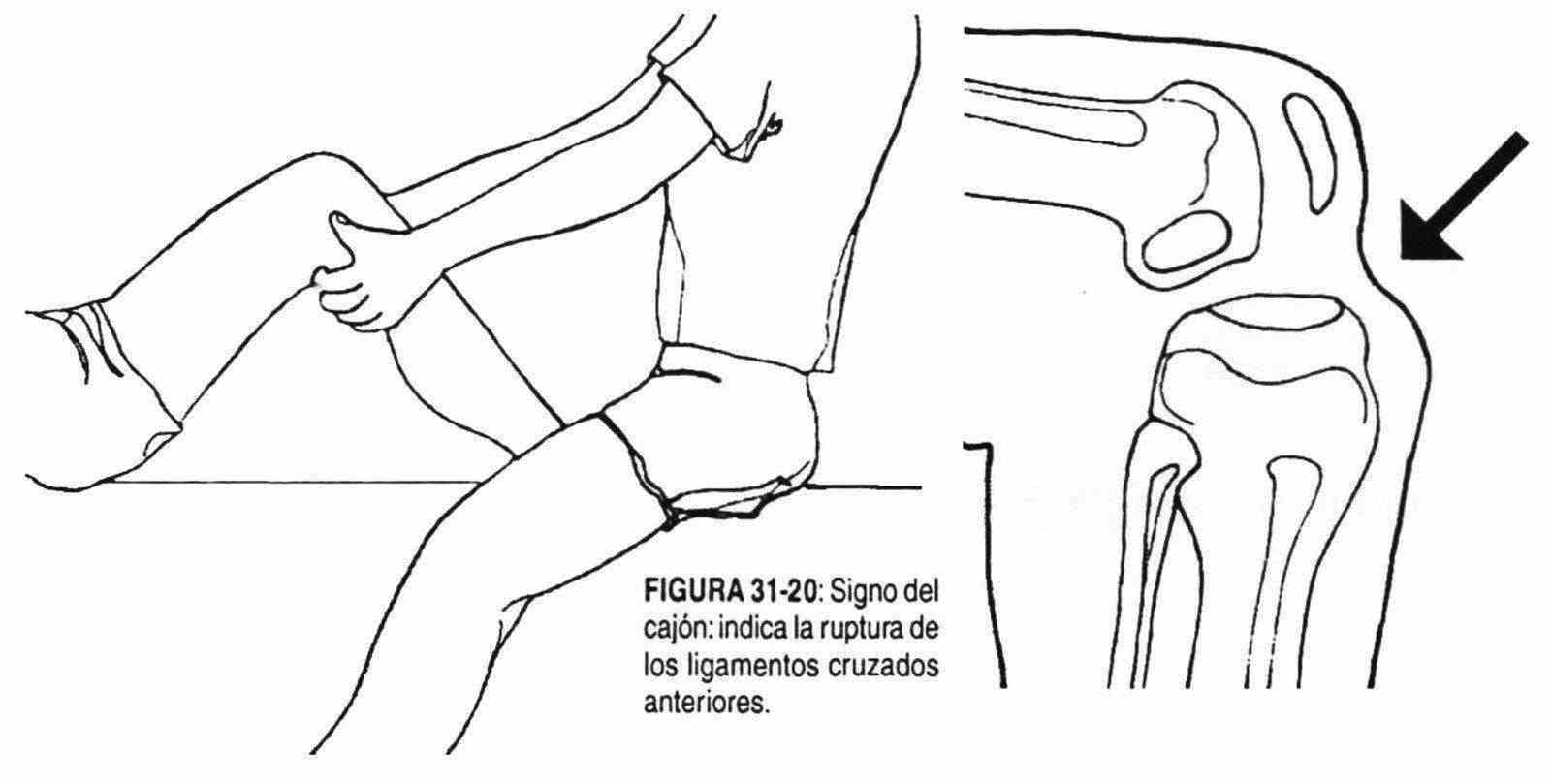
 Trauma to the knee is also common. A careful examination can reveal important signs of joint injury. With the knee flexed at 80 ° and the foot fixed on the stretcher, an attempt is made to bring the leg forward looking for an unevenness with a shoulder at the knee level, which indicates an injury to the anterior cruciate ligaments (box sign) (Figure 31 -twenty).
Trauma to the knee is also common. A careful examination can reveal important signs of joint injury. With the knee flexed at 80 ° and the foot fixed on the stretcher, an attempt is made to bring the leg forward looking for an unevenness with a shoulder at the knee level, which indicates an injury to the anterior cruciate ligaments (box sign) (Figure 31 -twenty).
Other times, with the leg fixed in extension, the examiner will try to perform internal and external lateral movements at the level of the knee, to rule out or check the existence of injury to the internal and external lateral ligaments of the joint that allow these abnormal movements (sign of internal and external yawning).
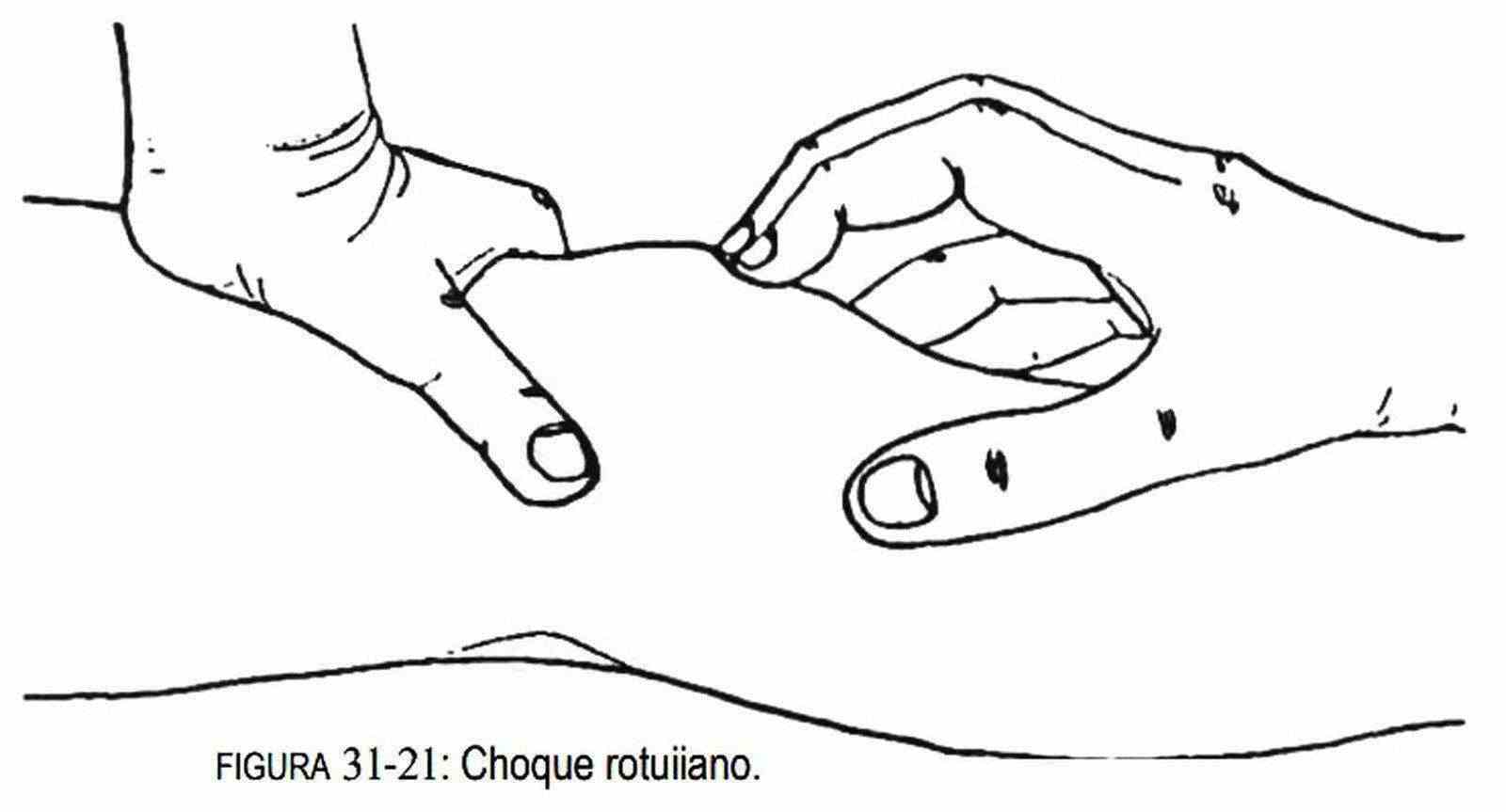
In addition, with the leg extended, and by compressing the periarticular serous bags with both hands, it will try - with the index of the hand that compresses the lower bags and pressing on the patella - to investigate whether or not there is an impact of the latter against the femoral condyles. (Figure 31-21). If positive, it is a sign that shows the presence of fluid in the joint cavity.
On some occasions, a superficial swelling is clearly delimited to the pre-patellar area, which indicates the presence of fluid in the pre-patellar bursa; this condition is frequent in the housewife.
Quadriceps atrophy, seen as a suprapatellar depression, is a sign of patella disease. Below the knee is the anterior tuberosity of the tibia, which can be found in young people and people who stay on their knees for a long time, painful and enlarged. It is the aseptic necrosis of the anterior tuberosity or Osgood-Schlatte disease.
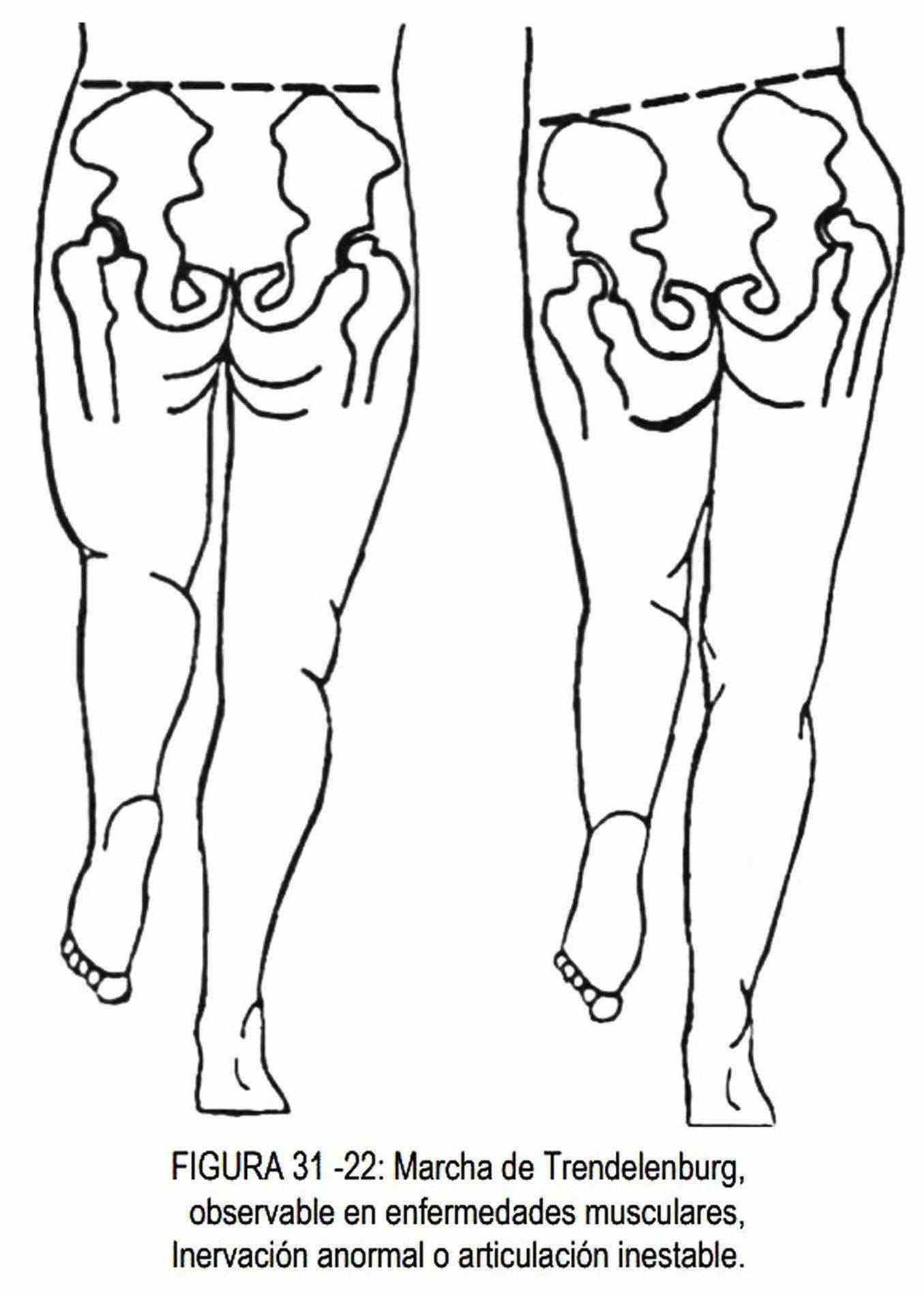
At the hip, the fall of the pelvis with gait to the side of the flexed limb is called the Trendelenburg gait (Figure 31-22), which means weakness of the abductor muscles due to muscle disease, absence of normal innervation, or a unstable joint.
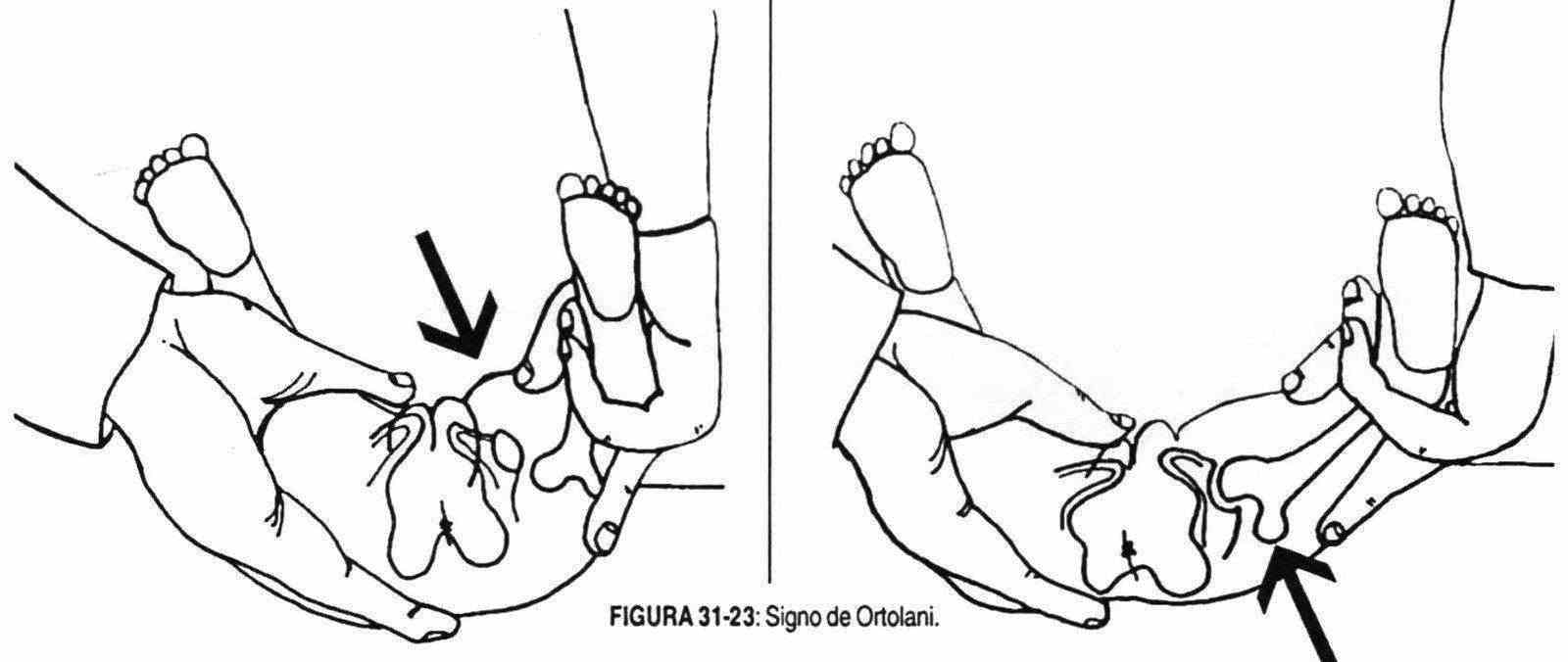
In the first years of life, more often in girls than in boys, it can be observed that one limb has less movement than the other, or that it is shortened, and that the hips are wider and the skin folds thigh are asymmetrical. In these cases, a limitation of abduction should be sought, which is investigated with the child lying down and with the knees and hips at 90 °; When the limbs are abducted, the separation obtained is less on the affected side. The Ortolani sign, audible, palpable and visible, is obtained with the same maneuver of separation of the limbs, at times when the femoral head passes over the posterior edge of the cup when attempting to separate. These signs are seen in congenital hip dislocation, better called congenital hip dysplasia (Figure 31-23).
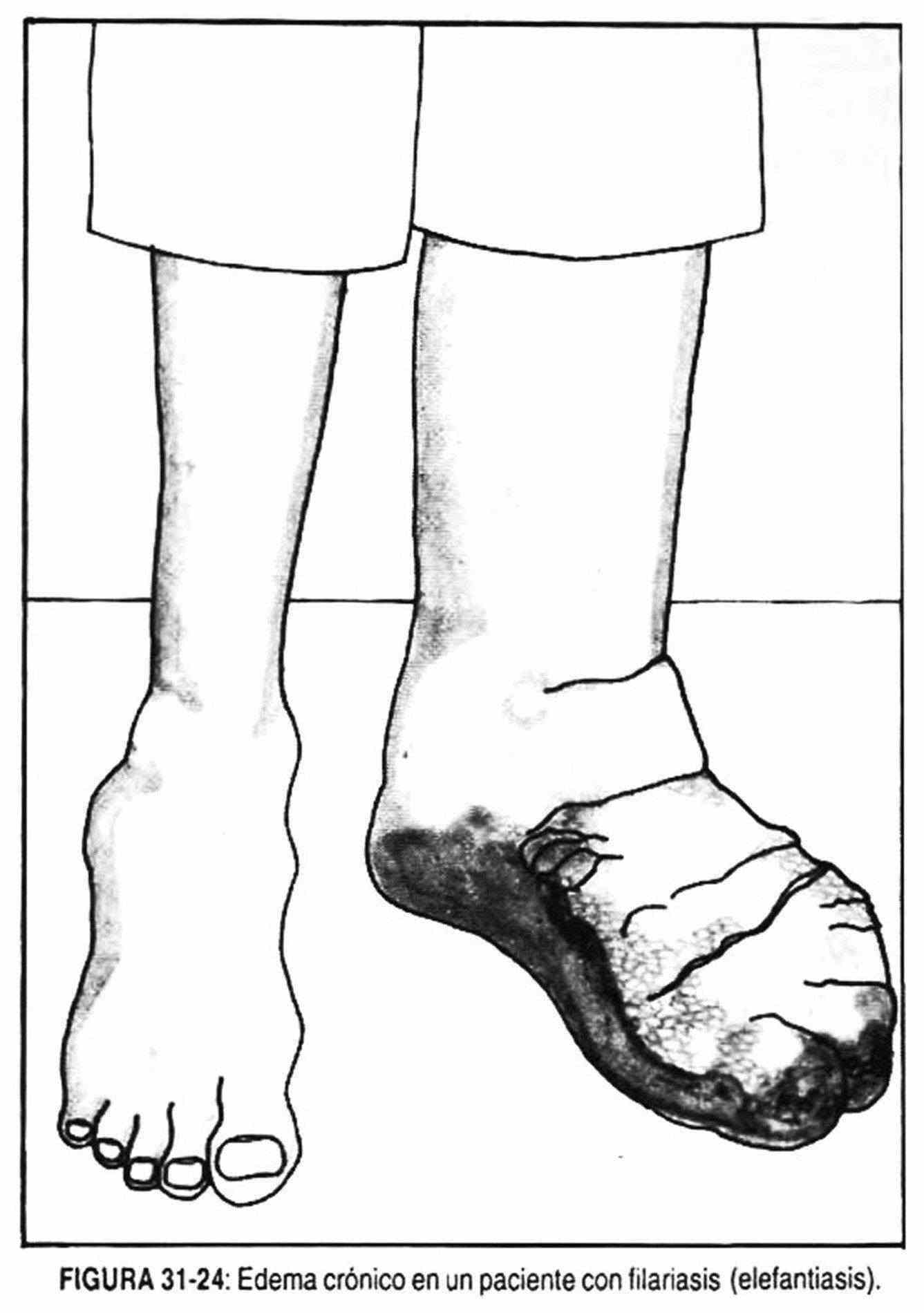
 Edema in the lower limbs . Swelling of the lower limbs or the presence of the Godet sign (impression left by the examining finger when pressing on the patient's pretibial region) uni- or bilateral, indicate the existence of edema. Edema can be locally caused or due to systemic diseases. Among the first, inflammatory processes and difficulties in venous and / or lymphatic drainage should be mentioned. In rare cases, edema is seen in patients with congenital malformations of the lymphatic tree (bilateral edema), as in Milroy disease, or is due to the presence of filariae in the lymphatic vessels (Figure 31-24).
Edema in the lower limbs . Swelling of the lower limbs or the presence of the Godet sign (impression left by the examining finger when pressing on the patient's pretibial region) uni- or bilateral, indicate the existence of edema. Edema can be locally caused or due to systemic diseases. Among the first, inflammatory processes and difficulties in venous and / or lymphatic drainage should be mentioned. In rare cases, edema is seen in patients with congenital malformations of the lymphatic tree (bilateral edema), as in Milroy disease, or is due to the presence of filariae in the lymphatic vessels (Figure 31-24).
Thrombophlebitis and varicose veins can cause edema in the affected lower limb. Lymphatic edema does not give the Godet sign (fovea). When the edema is bilateral, the most frequent causes are those of cardiac, renal or hepatic origin. Pediatric edema is occasionally observed in patients with subacute or chronic dermatitis of the lower limbs. This edema can be associated with chronic eczematous dermatitis and psoriasis and is not related to heart failure or lymphatic obstruction. Other times it is possible to observe a bilateral, hard, non-pitting edema with a decrease in temperature, corresponding to the edema of hypothyroidism. In hyperthyroidism, hard plaques of pretibial edema may also exist.
Alterations in the temperature of the lower limbs . They have already been described in the section corresponding to upper limbs.
Pain in the lower limbs . In some circumstances, at the level of the thigh and in the area innervated by the lateral cutaneous nerve of the thigh, the patient reports burning pain, with paresthesia. It occurs in individuals who wear corsets or belts with arms or who have pendulous abdomens, and it is believed to be caused by compression of this nerve as it passes under the inguinal ligament.
Ankle fractures can compress the posterior tibial nerve, causing tingling and pain on the bottom of the foot, which is tarsal tunnel syndrome.
Arterial disorders of the lower limbs . A careful medical history is important, not only because it directs attention to the affected limb, but also because it helps to evaluate, for example, the degree of evolution of an occlusive arterial process, and the development or not of a compensatory arterial circulation.
The increase, decrease or variation of symptoms and signs is the result of the evolution of these processes. The arterial system must be examined in its entirety, previously knowing which are the places that are most frequently affected; According to the medical history, it will begin with the supposedly normal area to end with the presumed pathological area.
 The absence or diminution of one or more of the normal pulses in the lower limbs can occur acutely or chronically, or be a finding on physical examination. Likewise, it is possible to auscultate murmurs at this level, as well as to observe cutaneous signs that are the result of the lack of oxygenation of the dermis.
The absence or diminution of one or more of the normal pulses in the lower limbs can occur acutely or chronically, or be a finding on physical examination. Likewise, it is possible to auscultate murmurs at this level, as well as to observe cutaneous signs that are the result of the lack of oxygenation of the dermis.
In a cold room, capillary flow is reduced and blood is diverted away from the skin; therefore, it is normal for it to appear pale and cold under such conditions. Vasoconstriction is more active in the lower limbs, and for this reason the feet may be colder than the hands.
In the examination of a limb with chronic arterial insufficiency, one or more of the following signs may be observed: lack of hair on the feet and hands, atrophy of muscles and soft tissues, transparent, shiny or friable skin, thickened nails with transverse and curved bridges longitudinally, with accumulation of cornified material below them, brown edema, coldness on palpation, and collapsed superficial veins.
Elevating the limbs and maintaining this posture actively or passively, produces
|
Table 31-1 Differences between chronic arterial insufficiency and chronic venous insufficiency |
|
|
Chronic arterial insufficiency
|
Chronic venous insufficiency
|
decreased coloration of the affected limb. If the circulation is normal, the pink color of the fingers will only be slightly reduced, whereas in arterial insufficiency not compensated by collaterals, a significant pallor will develop after 30 seconds of elevation.
The veins empty with elevation of the extremities, and under normal conditions they refill in less than ten seconds when they are lowered. Likewise, when a limb with arterial insufficiency is raised and then lowered, it recovers normal coloration in a time greater than ten seconds, as long as there are no varicose veins that allow retrograde filling. This filling will be delayed the greater the obstruction.
If there is chronic anoxia, flushing will develop that can take up to four minutes to reach its maximum intensity. When arterial insufficiency is suspected, it is important to observe the changes that occur with exercise, such as pale limb, disappearance of pulses, auscultation of murmurs in the great vessels that were not present at rest, and the appearance of pain. Long-standing severe ischemia produces rest pain that improves when the lower limb is placed hanging over the edge of the bed. The foot looks red and swollen, and unlike thrombophlebitis and cellulite, it is cold. In sympathectomy, whether surgical or spontaneous, as in the elderly, the skin is cold and dry, as in arterial insufficiency. The complete and acute occlusion of the artery produces,

 When the skin of the limbs presents areas of cyanosis and turns a purplish-black color that does not change with changes in position or with finger pressure, the limb may be pre-granular. This arterial insufficiency can progress towards necrosis of the limb tissues with mummification and desiccation, constituting grangrene. If infection is added, swelling, redness of neighboring tissues, and pain may be found.
When the skin of the limbs presents areas of cyanosis and turns a purplish-black color that does not change with changes in position or with finger pressure, the limb may be pre-granular. This arterial insufficiency can progress towards necrosis of the limb tissues with mummification and desiccation, constituting grangrene. If infection is added, swelling, redness of neighboring tissues, and pain may be found.
The absence or unevenness of the pulses at the level of the femoral artery, or the auscultation of murmurs, suggests the presence of aortoiliac occlusive disease. These murmurs represent turbulence caused by obstructions that prevent normal laminar blood flow. In complete obstruction of the vessel there is no murmur. When the obstruction is not complete, and there is no compensation for collateral circulation, a continuous murmur will be heard. Due to the tension gradient that exists, both in systole and diastole, the intensity of the murmur is not a reliable guide on the severity of the stenosis, since it is influenced by cardiac output, exercise, eventual anemia, etc. The irradiation of these murmurs follows the course of the blood vessels; are not very intense or disappear when the stethoscope is advanced towards the heart,
In a patient with unilateral varicose veins, a continuous murmur with a history of trauma is suggestive of arteriovenous communication. Other times, unilateral varices are observed with hypertrophy of the affected limb and superficial angiomas characteristic of Klippel-Trenaunay syndrome.
A unilateral increase in the amplitude of the femoral pulse may represent the increase in amplitude in an area of acute occlusion of this artery. This increase in amplitude is due to the fact that all the energy of the pulse wave is transmitted laterally at the point of occlusion. The most common area of occlusion in the femoral artery is the adductor or femoral duct, in the lower thigh region. Palpation of the popliteal artery requires experience and is often not palpable. In occlusive disease the pulse is absent. The posterior tibial artery pulse is only absent in very few normal individuals, so the fact that it is not found indicates, in general, occlusive vascular disease. The foot pulse may be absent in normal individuals.
Venous disorders of the lower limbs.
The venous system, especially that of the lower limbs, is frequently affected, giving rise to the so-called lower limb phlebopathies, which can be manifested by a wide variety of signs and symptoms, from a slight feeling of weight to functional impotence.
The term phlebopathy refers exclusively to the pathology of the venous system, without discriminating if it affects the deep, superficial or communicating system, or if they are combined forms.
When there are trophic disorders, no matter how small, they should lead to deep system disease, even when they coexist with visible superficial varices.
The dilations of the superficial veins of the lower limb are called varices. There are two types of varicose veins: primary, which are due to injury to the vessel wall or alteration of the venous valves, and secondary to obstructive processes of the iliofemoral vein or vena cava.
In the lower limbs there are two venous systems: the internal or greater saphenous, and the external or lesser saphenous. Both may be injured. The internal saphenous system drains at the level of the groin and the external saphenous 1 or does at the level of the popliteal fossa, being located posteroextema.
Both superficial systems are connected to the deep venous system by multiple communicating or perforating veins.

Pain is a frequent symptom with characteristics of heaviness and fatigue in the two lower limbs. It occurs in the standing position, increases with the passing of the day, and calms with the elevation of the limbs or ambulation. The discomfort increases during the spring and summer, and with menstruation. Sometimes the pain can be located in a venous tract. The edema is evening and diminishes or disappears with the decubitus; it is soft (and therefore leaves Godet) and can be unilateral or bilateral and not identical in both limbs. There are activities that are directly linked to the appearance of phlebopathies, such as those that require prolonged standing (dentists, shop assistants, cooks, etc.). In the interrogation, a history of pregnancy, childbirth and obesity should be sought,
Examination of the lower limbs for varicose veins should be performed with the patient standing up. If venous dilations appear, the examiner should take the following data into account:
 1. The presence of edema, ulcerations in the upper part of the internal malleolus, ocher pigmentation, and the presence of dermatitis (Figure 31-25).
1. The presence of edema, ulcerations in the upper part of the internal malleolus, ocher pigmentation, and the presence of dermatitis (Figure 31-25).
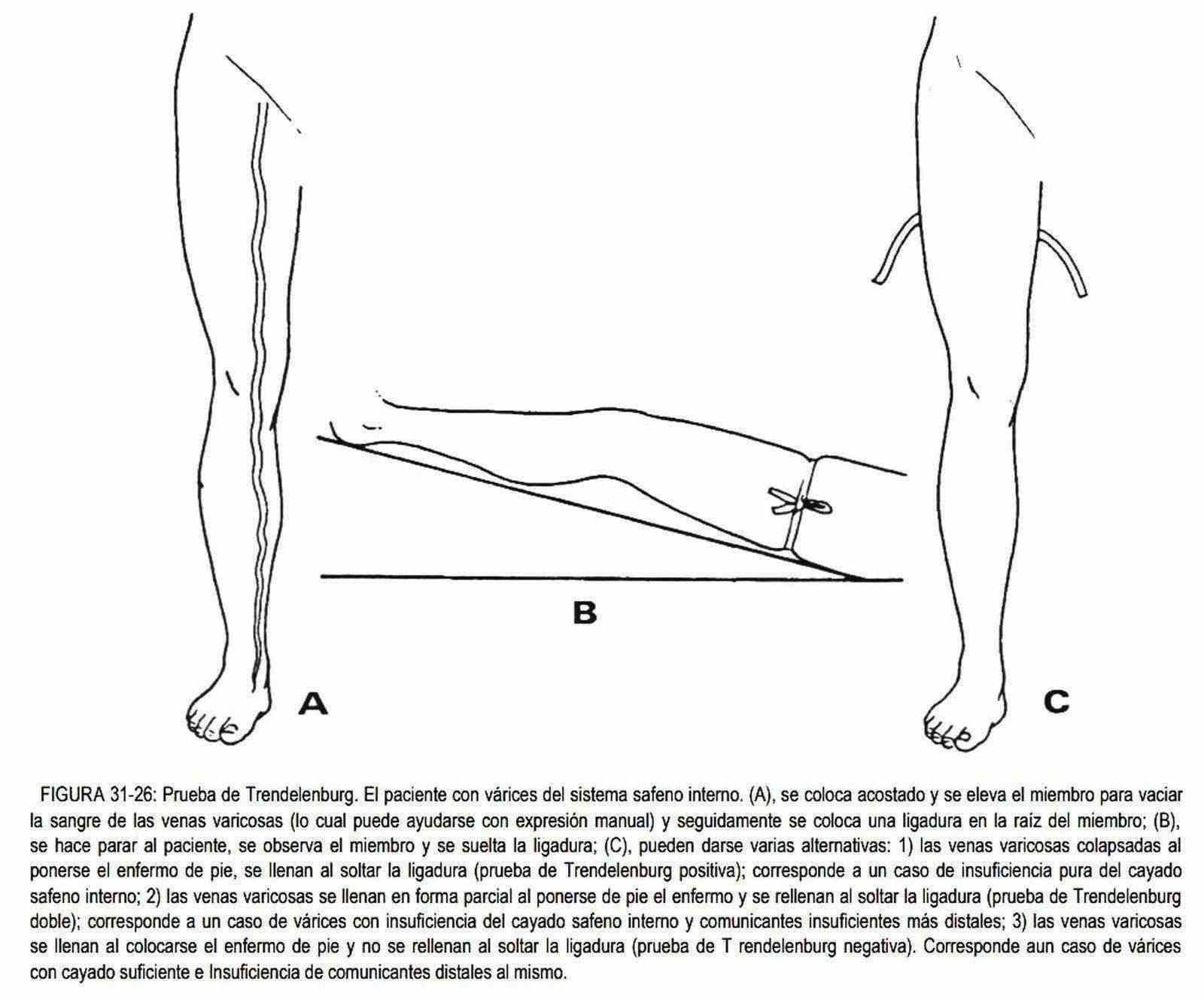
2. The indemnity or not of the communicating veins between the superficial and deep venous systems is investigated in the Trendelenburg test (Figure 31-26). The lower limb to be studied is raised, in order to empty the veins, and a tourniquet is placed on the thigh below the mouth of the internal saphenous vein. When resuming the standing position, if the veins of the communicating system are incompetent, they will fill and allow the filling of the veins of the superficial system, and if the latter fill more when removing the tourniquet, there will also be insufficiency of the saphenous arch .
As an additional maneuver, if the saphenous system has not been filled, it may fill abruptly when the tourniquet is released, indicating valvular insufficiency of the superficial or saphenous system.The Trendelenburg test can be performed partially or fractionally or with ligatures. multiple (one below the arch, the second above the femorotibial joint, and the third in the upper third of the leg). Later they are released in an ascending way, with the patient standing up, to try to locate which are the insufficient communicators.
Another way to evaluate the valves in this system is by the manual compression test, or the Schwartz maneuver (Figure 31-27). It is performed with the fingertips of one hand that compress and decompress the dilated veins in the upper part of the thigh, while with the other hand it is sought if the impulse is transmitted to a lower vein. If this occurs, it indicates valvular insufficiency of the saphenous system.
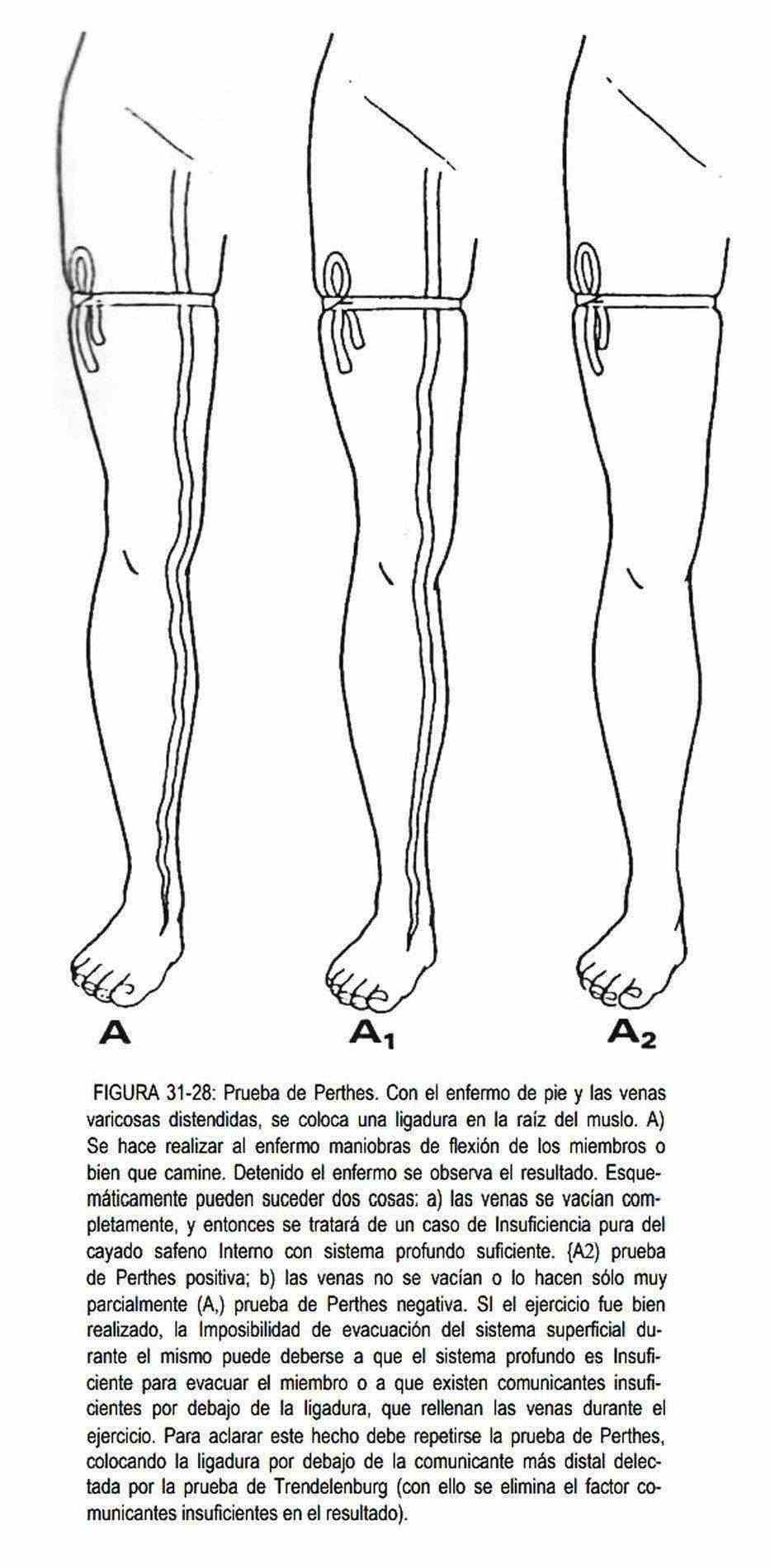
3. The degree of injury or indemnity of the deep venous system is assessed with the Perthes test (Figure 31-28). It is performed with a tourniquet that occludes the subcutaneous veins at the level of the thigh, below or at the level of the incompetent communicator. When the individual walks and the varicose veins fill below the tourniquet, he will be facing an incompetence of the deep system.
When combining the Perthes test with the Trendelenburg test, if the tourniquet is released below the last insufficient communicator located with the Trendelenburg test, and if the Perthes maneuver does not empty the varicose veins, it is in the presence of an insufficiency of the deep venous system.
4. The elastic bandage test, from foot to groin, with the veins empty in the supine position, provides valuable information about the deep venous system. The patient is asked to exercise, and if pain appears it is significant from deep system obstruction.
Venous thrombosis can be an acute process (thrombophlebitis) or a silent course (phlebothrombosis). Both can occur both in the superficial venous territory and in the deep system
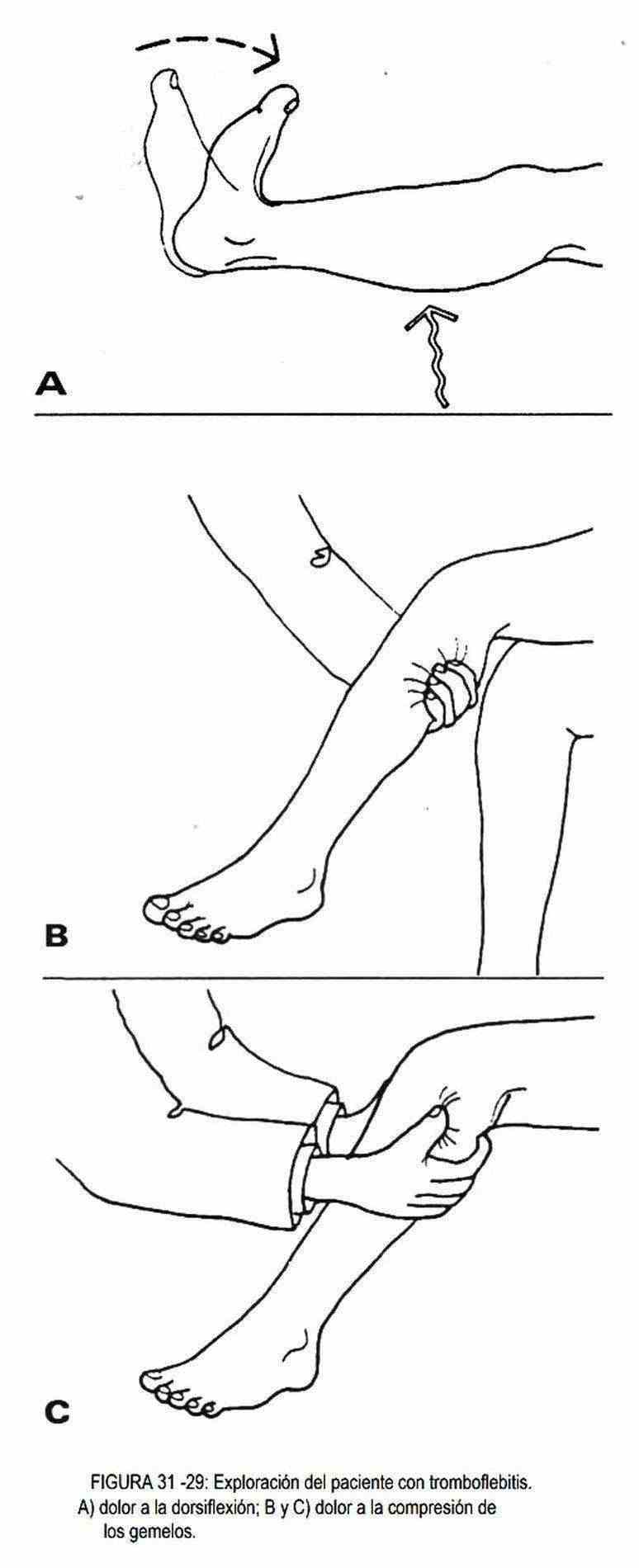
The signs of a superficial thrombophlebitis or phlebitis are the appearance of congestion or redness, induration, and the presence of pain. The swelling of the limb, together with a local increase in temperature, suggests the possibility of deep thrombophlebitis. The superficial veins are distended. Arterial pulses are preserved, although they may be diminished by reflex vasospasm. In these patients, compression of the calf is painful, and extreme passive dorsiflexion of the foot can cause pain at the level of the calves (Homans sign) (Figure 31-29). Uni or bimanual palpation of the calf can demonstrate the existence of a painful venous cord.
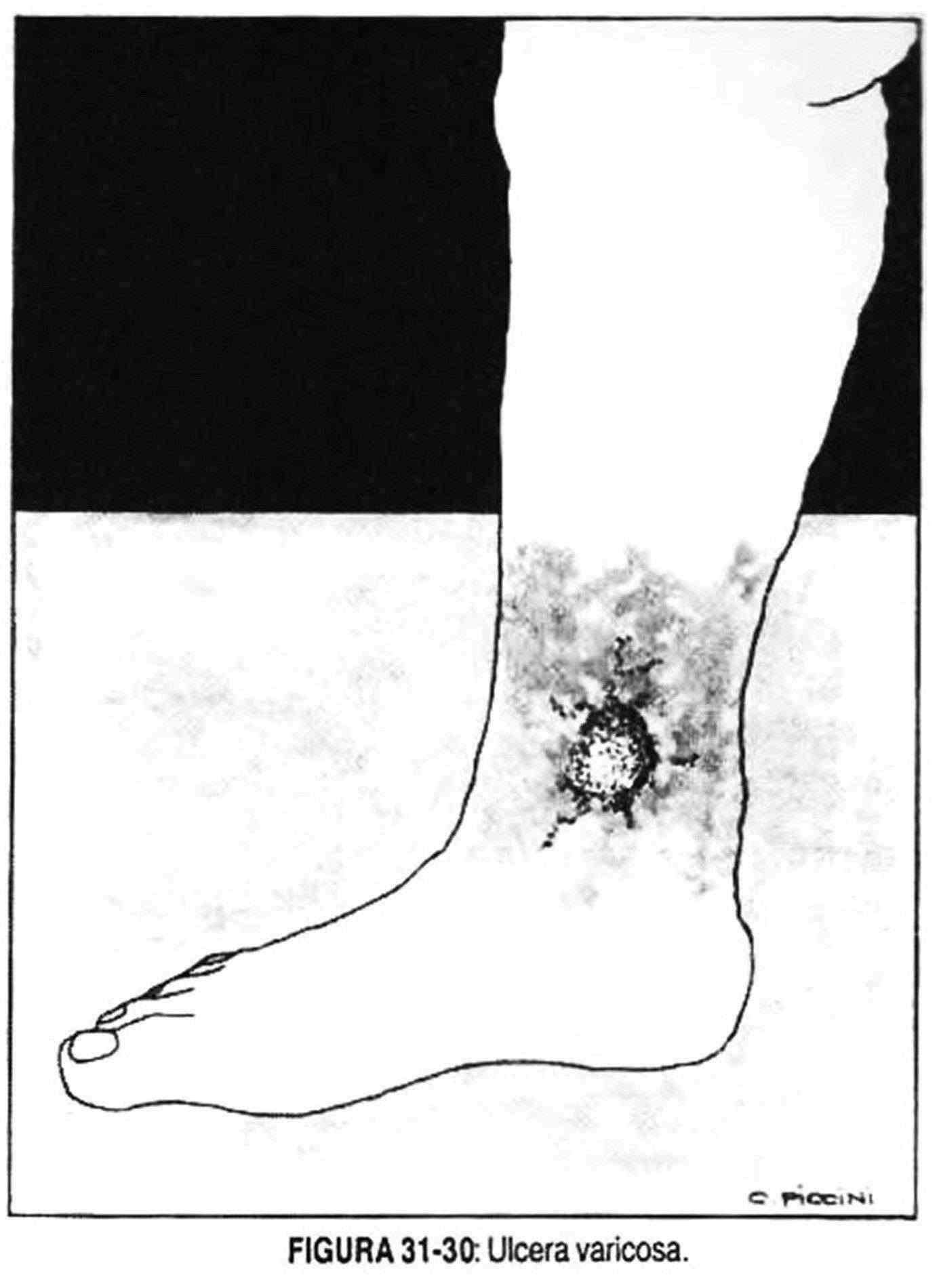
The painless, silent edema of overlapping evolution should make one suspect the possibility of deep thrombophlebitis. Palpation of the cellular tissue, if the skin slides freely over the aponeurotic planes or its mobility is limited due to fibrosis of the subcutaneous tissue, indicates the evolution of venous insufficiency or the existence of a postphlebitic syndrome. This syndrome is characterized by chronic venous insufficiency, which is evidenced by edema that gradually transforms into fibrous tissue, brownish skin due to extravasation of blood, pruritic eczematoid rash and an ulcer above the internal malleolus that is difficult to heal ( Figure 31-30).
 Skin disorders
Skin disorders
Erythema and / or peeling . Erythema and peeling of the skin on the hands and feet is a common disorder and may be due to contact with irritants and / or allergies, constituting contact dermatitis. Other times, there is erythema at the level of the flexion areas of the neck, the flexion folds of the elbow and the knee and wrists, with itching, which is observed in young people and represents atopic dermatitis. An erythematous area with small blisters, areas of vasculitis and an increase in local temperature, located in the lower limbs and with repercussions on the general condition, suggests the presence of erysipelas.
Thick, dry flaking without erythema, with the appearance of fish skin, affecting the entire body, although the palms and hands may be undamaged, constitutes ichthyosis. On other occasions, a scaly area or plaque is observed sitting on an erythematous area, which more frequently affects the skin folds, the elbows, the scalp, the buttocks and the tibial area, and which can be accompanied by alterations at the nail and articulate. This disease, not infrequently found, is called psoriasis.
Dry skin, with erythema and scaling, of universal distribution, is called generalized erythroderma, and can be seen in psoriasis and mycosis fungoides. When these lesions are localized, in the form of red or brownish plaques, which peel in a free or adherent form, in covered areas of the body, they may represent Bowen's disease, which is a carcinoma in situ, and must be taken into account for the differential diagnosis to arsenic injuries.
When the skin is normal and not thickened, erythematous and with a fine scaling, it is referred to as exfoliative erythroderma, which can be due to drug allergies, contact dermatitis or any inflammatory process of the skin, including leukemias and lymphomas. Another lesion characterized by erythema plaques with scaling is acrodermatitis enteropathica, which should not be confused with psoriasis. It begins with vesicles that evolve into scabs that become superinfected with Candida or other microorganisms. It can be hereditary in origin, in individuals in whom the thymus is absent, or seen in symptoms of malabsorption or in patients undergoing parenteral nutrition.
The presence of photosensitivity in childhood, with scars and hair loss, suggests the diagnosis of congenital erythropoietic porphyria; while the photosensitivity on the back of the hands, with fragility of the skin and the presence of vesicles, leads to suspicion of late hepatocutaneous porphyria.
Photosensitivity is observed in some aminoacidemias, as well as in Hartnup disease or tryptophan transport defect disease due to cellular nicotinamide deficiency. Phototoxicity does not respond to immune mechanisms. It is the reaction, when exposed to the sun, that is observed in patients treated with declomycin, sulfonamides, phenothiazines, thiazides, griseofulvin, etc., with the appearance of burning, erythema and edema, ending with scaling and hyperpigmentation. Photoallergy appears 24 hours or more after exposure to sunlight; it is persistent and is characterized by cross-photosensitization (sulfadiazine, sulfisoxazole). Other times, in areas exposed to sunlight, an erythematous, atrophic area is observed with pigmented spots that can evolve into a neoplasm,
 The presence of purple-blue macules or spots, which evolve into nodules, affecting the extremities and hands, and sometimes the face, is part of Kaposi's sarcoma. In the cold seasons and at the level of the distal parts of the extremities and on the ears, erythematous, itchy lesions may appear, which sometimes become infected and in others form blisters that later ulcerate. It is the so-called pernio erythema, more frequent in women.
The presence of purple-blue macules or spots, which evolve into nodules, affecting the extremities and hands, and sometimes the face, is part of Kaposi's sarcoma. In the cold seasons and at the level of the distal parts of the extremities and on the ears, erythematous, itchy lesions may appear, which sometimes become infected and in others form blisters that later ulcerate. It is the so-called pernio erythema, more frequent in women.
The interdigital folds can be erythematous, moist, with scratching lesions due to the presence of fungal processes, which in the foot are known by the name of athlete's foot.
Pigmentation disorders . The presence of spots or macules of circumscribed melanosis in areas exposed to the sun constitutes ephelides or freckles. These same lesions, but histologically different due to the increased number of melanocytes, which increase with age and exposure to the sun, are known by the name of senile lentigo.
Pigmentary moles or nevi, which appear as hyperpigmented, brown to black macules, sometimes have verrugoid or polypoid characteristics. Attention should be paid to changes in color, shape and size, as well as the appearance of ulcers and itching.
These changes indicate the need for a biopsy to rule out or confirm the existence of a melanoma, which is a tumor of the melanocytes, with great local and distant aggressiveness. Light skin and eyes appear to be predisposing factors.
Brown or black nevi, when they present red or white, grayish, pink or blue areas, should be examined histopathologically. Attention will also be paid to them when the edges are ragged, raised, or ulcerated. They are classified according to their clinical and histopathological features and are known as lentigo maligna, superficial spreading melanoma, and medullary melanoma. Nevi of the dermoepidermal junction, or junction nevi, are potentially malignant.
Changes in color and size and the presence of pruritus may indicate the need for a pathological study.
Sometimes pink macules can be seen on the limbs and trunk, preceded by hypopigmented ovoid lesions; when accompanied by sebaceous adenomas, mental retardation and seizures constitute the classic triad of tuberous sclerosis. The distinction between a depigmented area (tuberous sclerosis) and an apigmented area must be made with Wood's light.
The appearance of hyperpigmented, blackish-brown lesions with a velvety appearance constitutes acanthosis nigricans. This lesion is a frequent finding and can be a paraneoplastic manifestation of gastric, intestinal, mammary, prostate cancer. It can also be observed in hypercorticholémic obese patients.
The observation of reddish-brown macules that, when squeezed, produce local urticaria due to the release of histamine, with the formation of a papule, is a form of mastocytosis that occurs in children. Sometimes they accumulate to form nodules called mast cell tumors.
Squeezing them can cause flushing and colic.
Nodules . The presence of pedunculated tumors and subcutaneous nodules in the nerve tracts, together with café-au-lait spots, characterizes von Recklinghausen neurofibromatosis.
Bilateral painful erythematous nodules may appear on the anterior aspect of the tibia, and less frequently on the external area of the forearms, which are known as erythema nodosum. They can accompany rheumatic fever, streptococcal diseases, tuberculosis, leprosy, syphilis, sarcoidosis, the use of anovulatory drugs and sulfa drugs, ulcerative colitis and other chronic diseases.
It is also possible to observe erythematous and painful nodules, more frequent on the back of the legs and more rarely on the thighs, which can ulcerate and leave an atrophic surface. They constitute the indurated Bazin erythema and accompany vasculitis. The presence on the skin of firm or hard nodules, painless, erythematous or not, mobile, can be due to metastases of different neoplasms, such as breast, kidney, thyroid, lung, melanoma, stomach and rarely testicle, prostate and colon, and that can ulcerate as in leukemic and lymphomatous infiltrates.
Reddish nodules of 0.5 to 5 cm may also appear. in diameter in the lower limbs, or occasionally in other painful places, located in the subcutaneous tissue, which drain an aseptic fluid and are associated with pancreatitis and pancreatic cancer. It is the so-called liquefacing nodular panniculitis. It can be accompanied by polyarthritis, abdominal pain, and fever.
On other occasions, ulcerated nodules with translucent edges and telangiectasias are observed that constitute primary neoplasms of the skin. They are more common in fair-skinned subjects exposed to the sun or carcinogens, and usually develop on the face, although the limbs may be affected. The most common is basal cell epithelioma and later squamous cell epithelioma.
Those lesions with the appearance of indurated plaque, which progress by increasing in size over months or years, and which are characterized by presenting erythema and sustained desquamation, constitute mycosis fungoides or T-cell lymphomas, which originally affect the skin, but which they can be located in ganglia and viscera constituting Sezary syndrome.
There are also benign tumor nodules, such as soft subcutaneous lipomas that affect the back and limbs. When they are painful they constitute Dercum's disease.
Blisters . The presence of flaccid bullae on normal skin, which can be easily detached (Nikolsky's sign), especially on the trunk level, associated or not with lesions in the oral cavity, is suggestive of pemphigus. When the base is erythema cough and leaves concentric rings in the shape of a shooting target, erythema multiforme should be considered. They can also be observed in mucous membranes, are caused by vasculitis and can be associated with viral infections (herpes simplex, infectious mononucleosis, Mycoplasma pneumoniae, drug action, neoplasms.
Blisters with complete desquamation of the skin, sometimes periorificial in location, and involving mucosa, constitute the syndrome of epidermal toxic necrolysis or Stevens-Johnson syndrome; there is pluriorificial involvement and it can be secondary to the administration of drugs, such as sulfa drugs, neoplasms, viral diseases such as herpes, mycoplasma, and vaccinations.
Atrophic injuries . Circumscribed epidermal atrophy, leading to a transparent epidermis, occurs in discoid lupus erythematosus. Among the atrophic lesions are those that affect exposed areas of the limbs, both lower and upper, which begin as small, painless and nodular lesions, with circumscribed edges, which increase in size, flatten and depress when the skin it atrophies, and they can ulcerate. These lesions are known as lipoid necrosis diabeticorum and can appear even before the symptoms and signs of diabetes mellitus are present. They are seen more frequently in women, affect the lower limbs more often, and are generally related to minor trauma in the area.
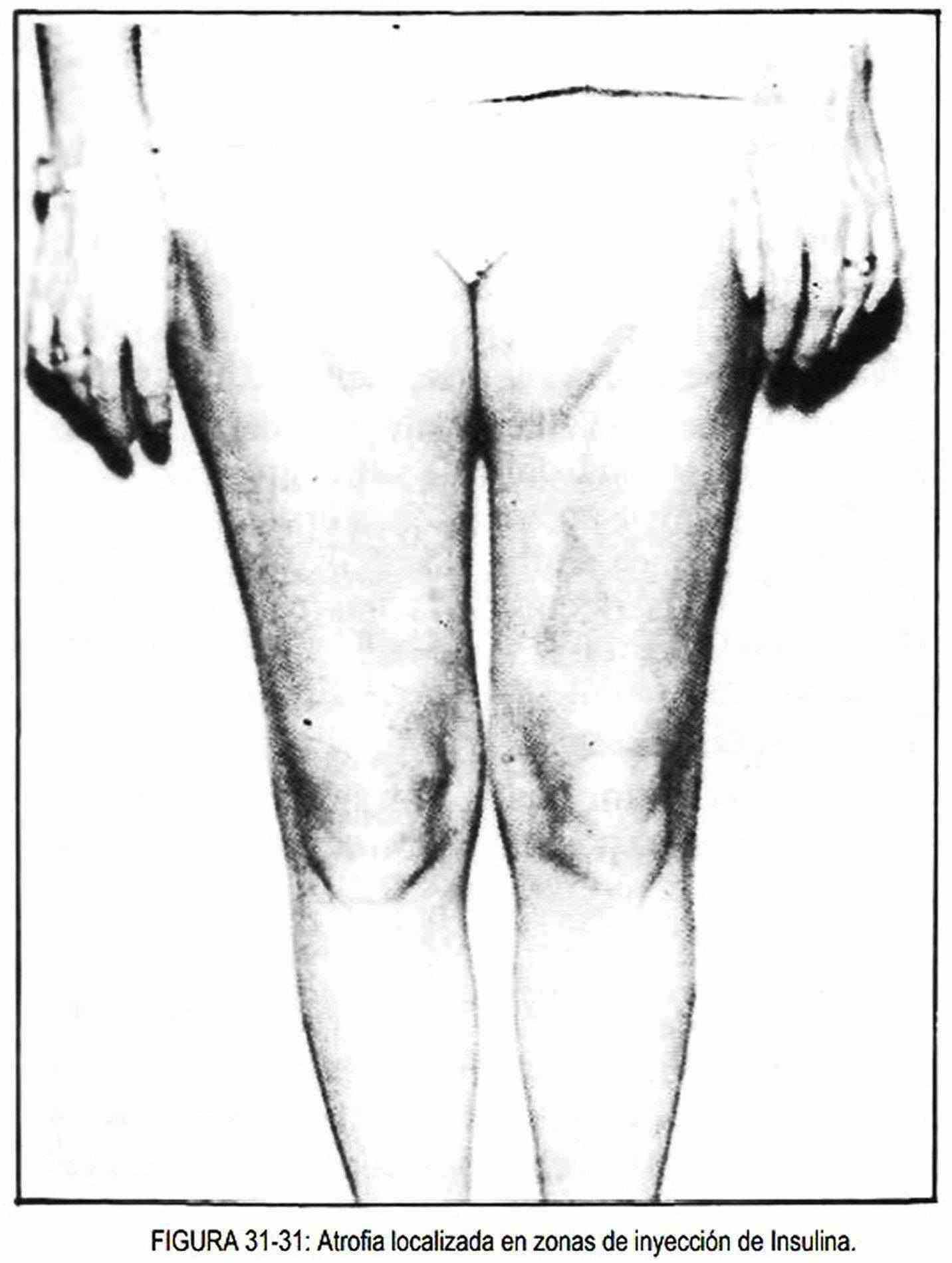
The use of insulin can produce lipodystrophic lesions (Figure 31–31), with areas of atrophy and hypertrophy of adipose tissue, which are seen more frequently in adolescent girls and at sites of insulin application.
The presence of sclerosis plaques, with white or yellowish centers, and lilac telangiectatic borders, constitutes a localized or circumscribed form of scleroderma, without another systemic involvement, called morphea.
Thickening of the skin . At the level of the bony prominences of the foot, for example, in the fifth toe, chronic, painful thickening of the skin can occur, with the pointed end directed towards the dermis. They are known as a rooster's eye. Non-painful thickening, called corns, develop on other pressure areas where the skin is thicker.
If there is pain, the existence of a wart under the callus can be suspected. The plantar wart looks like a callus, or it may be covered by a callus; it presents small spots that give it a mottled appearance and is located in the cutaneous thickening of the sole of the foot; skin lines stop at the edges of the wart (Figure 31-19, C).
 Ulcerated lesions . On the skin of the limbs it is possible to find ulcerations that are sometimes accompanied by nodular lesions and regional lymphadenopathy, and that can be seen in primary syphilis and tuberculosis, bubonic plague and tularemia, anthrax. In isolation they are seen in cryptococcosis, sporotrichosis, leishmaniasis, and tertiary syphilis.
Ulcerated lesions . On the skin of the limbs it is possible to find ulcerations that are sometimes accompanied by nodular lesions and regional lymphadenopathy, and that can be seen in primary syphilis and tuberculosis, bubonic plague and tularemia, anthrax. In isolation they are seen in cryptococcosis, sporotrichosis, leishmaniasis, and tertiary syphilis.
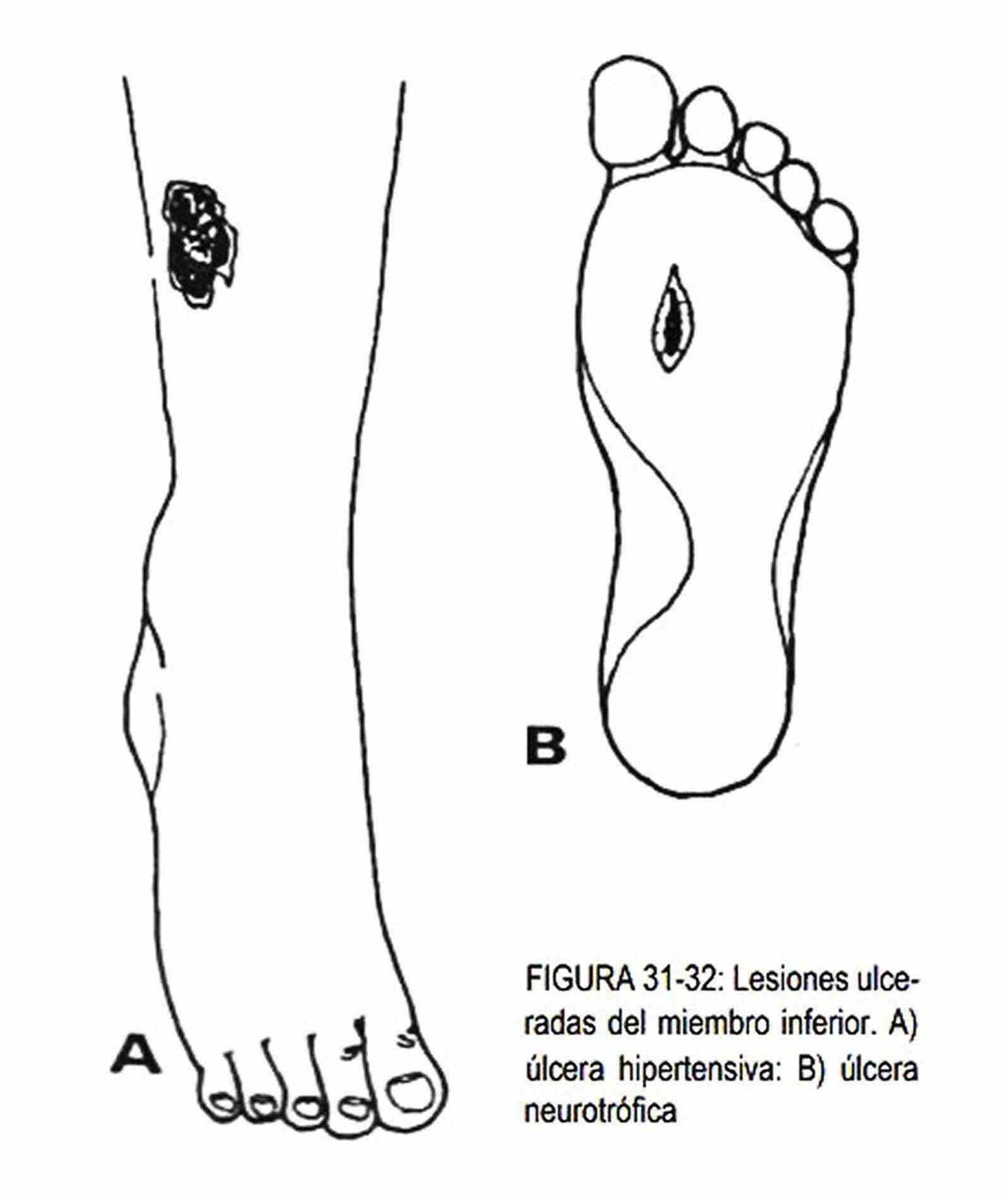
In the middle of the ankle or in the lower and inner end of the leg, the presence of ulcers on a pigmented ocher-brown skin, with edema and areas of retraction, and varicose dilations in the lower limbs, is frequent in insufficiency chronic venous. On the lateral side of the ankle, neat border ulcerations (Figure 31-32, A) may accompany hypertensive disease, vasculitis, renal failure, systemic lupus erythematosus, Raynaud's disease, and cryoglobulinemia.
When the ulcer sits on a necrotic base, bluish-red in color, with multiple, irregular and protruding edges, and which can cover extensive areas of the lower limb, it is the pyoderma gangrenosum ulcer, frequently associated with Crohn's disease and ulcerative colitis.
Neurotrophic ulcers (Figure 31-32, B) occur at pressure sites on the feet, where there is decreased or absent sensation, as occurs, for example, in diabetic and alcoholic neuropathies. They are deep, painless ulcers and may be infected.
Within Mushausen's self-harm syndrome, factitious ulcers produced by cigarette or acid burns can be seen. Other times leg ulcers accompany blood diseases, such as anemia, hemolytics, sickle cell disease, thalassemia, and hereditary spherocytosis.
Hemorrhagic lesions . In certain haemorrhagic diseases, it is possible to observe pinpoint-sized, red-colored lesions on the skin that do not disappear with vitro pressure and are called petechiae.
They are caused by an alteration of platelets in their number or function. Ecchymoses are larger hemorrhagic suffusions; vines are linear hemorrhages, which are sometimes produced by scratching in patients with itching and coagulation disorders.
The appearance of twenty or more petechiae after adjusting the cuff below the maximum blood pressure, but above the diastolic pressure for a few minutes, is called Rumpell-Leede phenomenon and is seen in capillary or blood disorders. hemostasis.
Other skin lesions . Occasionally, small papular lesions measuring 1–2 mm, similar to goose bumps, may appear in the armpit and neck, constituting the elastic pseudoxanloma. It is an inherited, recessive disorder that affects the skin, eyes (visual disturbances, blindness), and the vascular system (bleeding at any level).
Neurological disorders
The neurological examination of the limbs assesses muscle strength and trophism, different types of superficial and deep sensitivity, the existence of normal reflexes or the appearance of pathological reflexes, muscle tone, the presence of abnormal movements, coordination of movements and the march. All these aspects are covered in Chapter 32.
Muscular system disorders
Palpation of the lower and upper limbs is used to detect abnormalities in muscle tone and sensitivity.
The alterations of the muscular masses can appear in acute, subacute or chronic form or in episodic form, and present with muscular weakness or paresis or paralysis. They can also do it with muscle pain, spasms, cramps and localized muscle tumors.
Among the acute, subacute pictures, there are some collagen diseases (dermatomyositis-poliomyositis), infectious diseases such as botulism, viral diseases such as poliomyelitis, or toxic diseases such as organophosphate poisoning. Chronic symptoms include muscular dystrophies, Duchenne type (ape hand), Landouzy-Dejerine type (facioscapulohumeral), in hyperthyroidism, or Charcot-Marie-Tooth type (muscular atrophy, usually of the peroneals). There are also other clinical entities that present with chronic muscle disorders (leprosy, sarcoidosis, arsenic poisoning, alcoholism, diabetes, polyneuropathies, amyloidosis).
Among the episodic paralyzes, myasthenia gravis, familial periodic paralysis, and also hyperthyroidism should be mentioned. Among the myalgic conditions, those of trichinosis, polymyalgia rheumatica, polymyositis and other collagen diseases that are accompanied by muscular inflammatory processes are characteristic. In turn, localized muscle tumors may be due to rupture, muscle hemorrhage or muscle tumors (rhabdomyosarcoma, angioma, metastasis), and the presence of granulomas (sarcoidosis, tuberculosis) and pyogenic abscesses.
Among the pictures that present with rigidity, spasms and cramps, are tetanus, tetany and Thomsen's disease. Other times muscle atrophy is caused by starvation, neoplastic cachexia, or by drugs (corticosteroids, vincristine).
Pathological alterations in muscle volume must be distinguished from the normal differences that exist between men and women and from those due to muscle development caused by the predominant use of certain muscle groups. The congenital myotonia seen in circus exhibitionists, or that seen in pseudohypertrophy, such as Thomsen disease, are examples of increased muscle volume.
Examination of mobility should be performed by localized muscle groups, one by one, to detect focal alterations. General mobility will then be assessed to investigate universal anomalies. The limb examination will continue by requiring the lying patient to raise the lower limbs 45 °. This maneuver is intended to evaluate muscle response. He is then instructed to close his eyes to avoid ocular correction of mobility abnormalities.
The upper limbs will be subsequently evaluated. The seated patient is asked to raise the limbs to 90 °, and then keep them elevated with the eyes closed. After performing these maneuvers, the examiner must counter these movements to detect abnormalities in muscle strength.
