Monica Espinoza
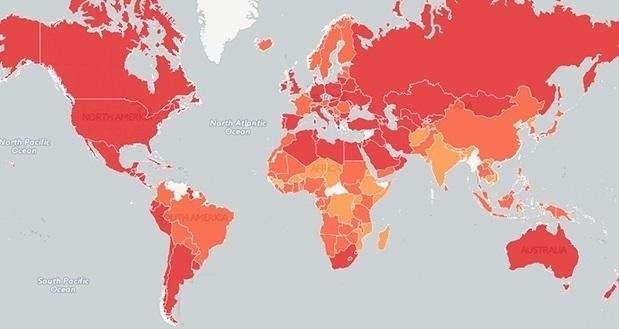
Obesity is an increasingly frequent syndromic disease, a pandemic that has been on the rise since the mid-20th century but in the 1980s it showed a marked and striking increase.
The increase in its prevalence led to the talk of the global obesity epidemic, being the first time that a metabolic, chronic and non-communicable disease is considered an epidemic. (CNCD)
Data taken from WHO
- In 2016, 39% of adults aged 18 and over (39% of men and 40% of women) were overweight.
- Overall, in 2016 around 13% of the world's adult population (11% of men and 15% of women) were obese.
- Between 1975 and 2016, the global prevalence of obesity has almost tripled.
- The same problem is seen in children and adolescents. In 2016, more than 41 million children under five years of age worldwide were overweight and obese
It is heterogeneous because we can speak of obesity because it occurs in different ways in terms of the location of the fat deposit, but this increase in the fat deposit that defines obesity is not always accompanied by physical symptoms or comorbidities. It is a set of symptoms and signs (Syndrome) and in turn has markers that allow its diagnosis as a disease.
When it is not accompanied by symptoms, can we then speak of healthy obese? . To answer affirmatively to this question would be to ignore the classification of obesity that takes into account the predominantly medical forms and the predominantly cultural ones, or to put it another way, a way not related to physical health, but what makes the social outlook sick. Discrimination suffered by those who do not have a socially accepted weight.
The following map is the WHO publication showing levels of overweight and obesity in the world based on information from 193 countries obtained in 2014.
 Definition
Definition
Obesity is an epidemic, metabolic, chronic, heterogeneous and stigmatized disease, of multifactorial origin, characterized by excess body fat (CG), the magnitude and distribution of which determines the health of the individual and is determined by the interaction of genetic and health factors. medium (hypercaloric / hyperfat diet and sedentary lifestyle). - [i]
This increase in CO is frequently accompanied by an increase in body weight (CP). The magnitude, the distribution with ectopic fat deposition and the hypertrophic character will be the determinants of the degree of disease and the appearance of its comorbidities.
This body fat (CG) can be estimated with simple and accessible methods such as bioimpedance or with Densitometry or Hydrodensitometry considered the gold standard to measure CG.
Table 1 Criteria for normality and obesity
|
Category |
Mens % |
Women% |
|
Normal |
12-20 |
20-30 |
|
Limit |
21-25 |
31-33 |
|
Obesity |
>25 |
>33 |
As clinical semiologists we need a definition that allows the diagnosis:
Overweight BMI 25 to 29.9
Obesity Grade 1 BMI 30-34.9
Grade 2 35-39.9
Grade 3> or equal to 40
Another parameter to take into account in the diagnosis is the perimeter or waist circumference (WC) that will depend on the ethnic groups according to the consensus of the International Diabetes Federation (IDF) 2005.
Central obesity.
-CC H >94 y M>80 europids
H> 90 and M> 80 South Asia-America
central and south
M> 85 and M> 90 Japan
This is explained by the difference in body composition, for example Asians with a lower BMI may have a higher proportion of GC, whereas blacks have a greater bone and muscle structure than other races, with a higher BMI having a lower proportion fat. [ii]
Causes
To understand the causes of this epidemic, it is necessary to refer to different theories.
Homo sapiens competed with other species and with severe climatic conditions, being a hunter-gatherer who understood that when there was food, it was necessary to eat, if it was fat, better because this allowed him to treasure to be able to face periods of scarcity. This caloric excess is deposited in the form of fat.
This is the thrifty genotype theory [iii] (Neel) of prehistoric man
If you think about the history of humanity, you can see that there were great changes in food. This concept of nutritional transition [iv] is what explains the transition from a diet eminently coming from agriculture and livestock to that which appears at the end of the 18th century with the industrial revolution. This allowed greater development of food together with greater economic availability, consequently producing an increase in the consumption of calories and fat.
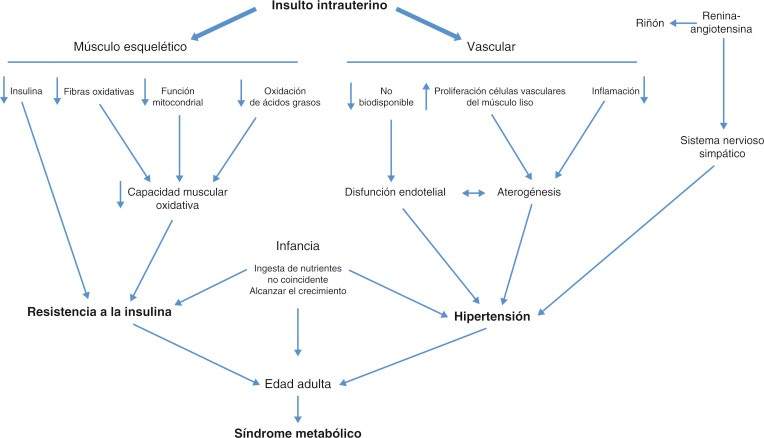
The Theory Barker associating fetal malnutrition low birth weight to the trigger to be a generate insulin resistance. The fetus can adapt to malnutrition, altering its hormonal production or the sensitivity of tissues to hormones, and also redistributing blood flow to protect the most important organs such as the brain. This insulin resistance predisposes to obesity but fundamentally to central obesity associated with insulin resistance with glucose intolerance, dyslipidemia and arterial hypertension. [v]
The following graph (1) explains the sequence of this process [vi]
If to these fundamentals is added a great availability of foods, rich in fats, sugars and salt, intense advertising to increase consumption, larger portions, plus a growing number of screens (televisions, computers) that promote sedentary lifestyle, the indispensable medium is generated obesity, thus culminating in the growing and unstoppable at least so far) obesity epidemic.
Pathophysiology
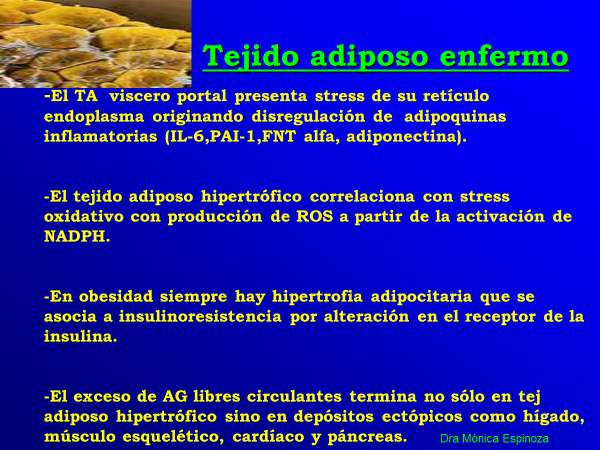
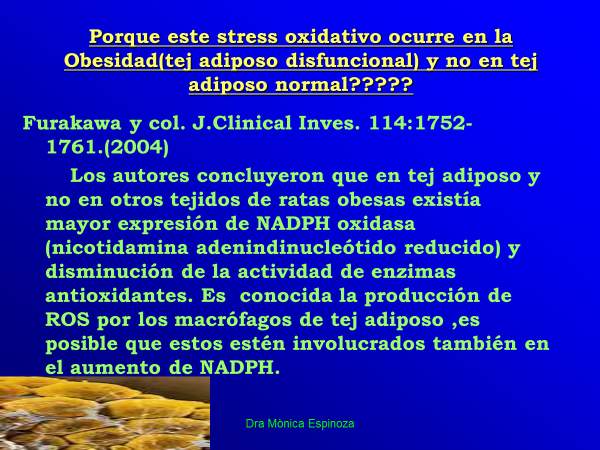
You can start by accepting that obesity is the product of an imbalance between food income and energy expenditure. When the relationship between these variables generates a positive balance, an increase in fat deposits is generated, that is, an increase in the number of adipocytes (hyperplasia) but especially adipocyte hypertrophy, which is the genesis of the pro-inflammatory state of obesity.
The question we must ask is why do we eat?
Eating behavior includes a psychobiological process since there is a need for energy input on the one hand and also a hedonic process in the search for pleasure and reward through ingestion. A third component is the stress system that prepares for the fight, defense or flight with the release of appropriate hormones.
There is a consensus on the existence of a physiological mechanism whose function is to keep energy reserves in balance according to nutrition and energy expenditure demands.
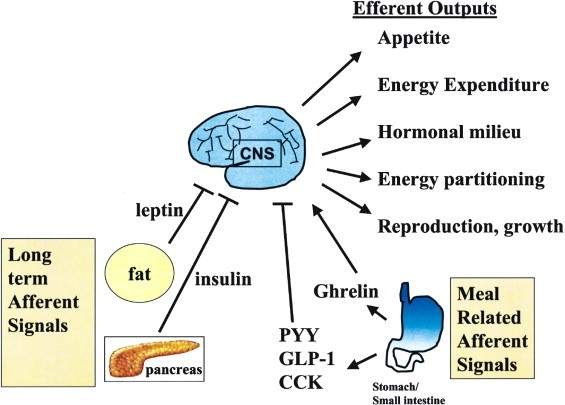
This system has both afferent and efferent signals.
The afferent signals inform about the start and end of an individual intake (short term) and also give information about the state of reserve storage (long term).
Graph 2 shows the short-term afferent signals that stimulate ingestion (Ghrelin), those that inhibit it (PYY, GLP-1, CCK) and those of the long term (Insulin, leptin). While the efferent signals regulate appetite and energy expenditure.
The afferent signals carry their information to the brain center of the hypothalamus from where a response to these signals will be generated [vii].
The biggest drawback is that this system is more prepared to generate a response to intake and storage deficits than to excess energy. The thrifty gene prepared us to survive in times of deficiency, therefore the circuits that suppress appetite and increase energy expenditure to prevent obesity, are insufficient.
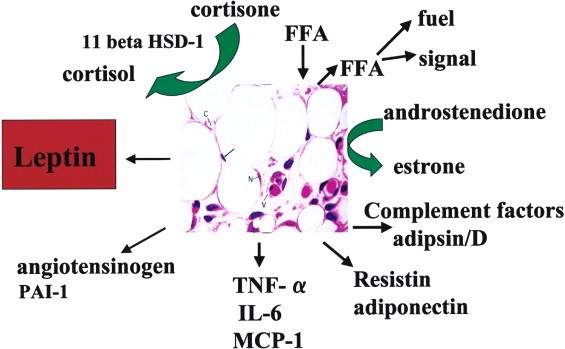
To begin with the physiopathology of obesity, the fundamental role of the adipocyte must be understood, storing excess energy in the form of triglycerides and releasing them in times of need.
The adipocyte releases about 600 adipokines, of which leptin and adiponectin are the most studied and known. Adipose tissue is made up not only of adipocytes but also by connective tissue where the macrophages responsible for the release of inflammatory cytokines are found
The adipocyte as an endocrine cell (Obesity Wars. Review Cell vol 116 2004)
 In obesity, it is observed that adipose tissue develops through hypertrophy when it is subjected to a hypercaloric diet and then when it reaches its maximum growth threshold, hyperplasia begins. [Viii]
In obesity, it is observed that adipose tissue develops through hypertrophy when it is subjected to a hypercaloric diet and then when it reaches its maximum growth threshold, hyperplasia begins. [Viii]
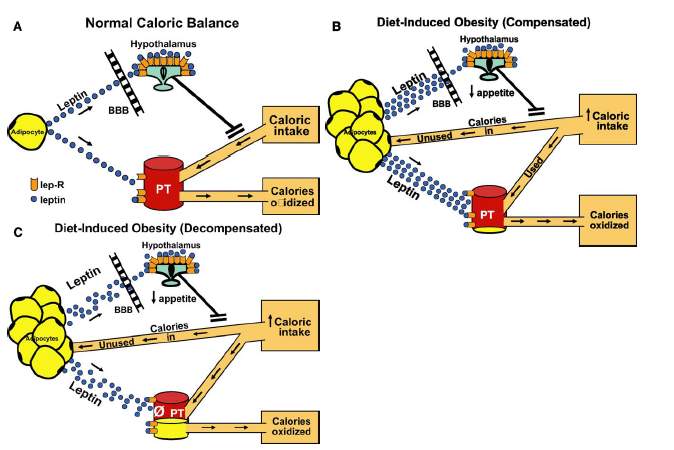
The following graph [ix] (3) helps to understand how, with a normocaloric diet, adipose tissue releases leptin that acts on its receptor (lep-R) in the hypothalamus, inhibiting intake. Thus the ingested calories are in balance with the oxidized ones, not producing fat deposition in peripheral tissue (TP).
When caloric intake increases, adipose tissue hypertrophy and hyperplasia occur, leptin levels increase that promote a decrease in intake, but it also acts on TP, favoring the oxidation of fatty acids. This is enough to avoid fat deposition in peripheral tissues while diet-induced obesity is compensated. If you continue the hypercaloric diet, and even with higher levels of leptin, the deposit of fat in peripheral tissue will be even greater, also producing a resistance to the action of leptin at this level.
Initially, adipocyte hypertrophy generates a mild inflammatory state, but if the conditions are perpetuated, apoptosis (adipocyte destruction) and generation of inflammatory factors are generated that pass into the circulation, generating a low-grade systemic inflammatory state.
The hypertrophied adipocyte (diseased adipocyte) and the inflammatory state generated by macrophages of the adipose tissue generate insulin resistance
The accumulation of intraadipocyte triglycerides produces the degradation of the insulin receptor, this prevents the transfer of the glucose transporter into the cell (Glup 4) towards the cell membrane and thus the appearance of hyperglycemia.
This larger size of the adipocyte increases the production of leptin but also decreases that of adiponectin, which has a protective effect against insulin resistance, generating mitochondrial stress and impaired mitochondrial function.
As seen in Figure 3, in decompensated obesity, fat deposition begins in other tissues (ectopic fat deposition), further promoting insulin resistance.
Eating behavior
Leptin as an afferent signal reaches its receptor in the hypothalamus, informing about the levels of peripheral fat deposits. This produces the release in the arcuate nucleus of anorectic substances such as POMC (Propiomelanocortin) and CART (cocaine and amphetamine regulated transcript) and in the intestine to peptide YY (PYY), and inhibiting the release of NPY and AgRP, orexigenic substances.
Under negative balance circumstances, there is a drop in leptin levels and gastric secretion of ghrelin increases, which acts on AgRP, inhibiting the release of POMC. This would lead to an increase in intake to reconstitute energy levels. [X]
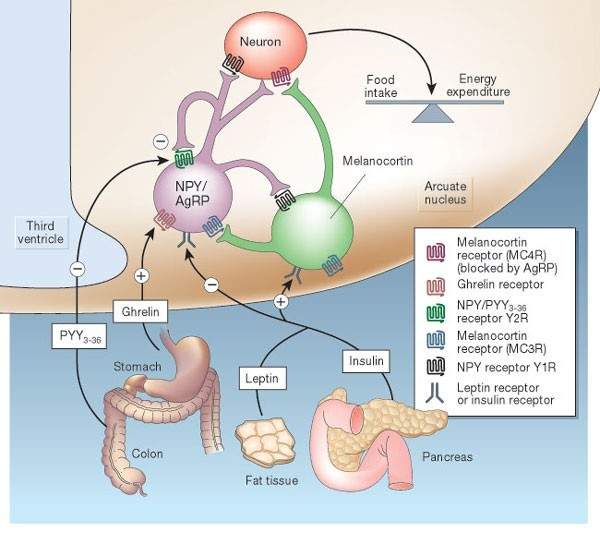 The following graph [xi] shows how the different central and peripheral neurotransmitters interact in the regulation of food intake
The following graph [xi] shows how the different central and peripheral neurotransmitters interact in the regulation of food intake
Semiology in the obese patient
You should start with the Clinical History taking into account that it should always be complete as in all cases.
As Reasons for Consultation in these patients can be found for example:
Cardiovascular system: Uncontrolled hypertension, dyspnea, palpitations, lower limb edema
Respiratory System: Sleep apneas, snoring with associated daytime sleepiness.
Gastrointestinal System: Heartburn, gastroesophageal reflux many times with associated cough
Locomotor system: Pain in lower extremities due to knee osteoarthritis, presence of peripheral varicopathy and edema of both legs often associated with Erysipelas.
Endocrine: Diabetes difficult to control, dyslipemia
Skin: Erysipelas, mycosis of submammary folds, epiploic apron, inguinal
Within the Personal Background and Habits you should look for:
- age of onset of overweight
- history of treatments or not for weight loss
- weight curve
- eating habits
- sleep characteristics to check for snoring or apneas such as the origin of arterial hypertension or arrhythmias
- use of drugs that can cause weight gain. Ex: insulin, corticosteroids, lithium, tricyclic antidepressants, thiazolidinediones
- physical activity
Always look for comorbidities associated with obesity such as diabetes, hypertension, dyslipidemia, hyperuricemia, cancer, gallstones, coronary heart disease, cerebrovascular accidents.
As a Family History, it is important to know a family history of obesity, especially morbid obesity, which will give us an idea of probable genetic obesity (rare as Prader Willi) or bad family eating habits, that is, an obesogenic environment.
Physical exam
Among the vital signs, high blood pressure can be found frequently.
Always when weighing and measuring our patients, we will calculate a BMI that will be equal to or greater than 25. In addition, waist circumference should be measured where, for the cardio-metabolic risk to increase, it must be greater than or equal to 80 cm in women and greater or equal to 94 in men.
Also bear in mind that on some occasions you can find individuals at the limit of normal weight or slightly overweight but with altered abdominal circumference who behave as metabolically obese of normal weight.
The obese patient may have a tendency to sleep since it is the high prevalence of snoring and sleep apneas that cause daytime hypersomnia as well as arrhythmias and arterial hypertension.
Continuing with the inspection, observe the skin, of thighs more frequently, with a characteristic poceado (orange peel).
Look for acanthosis nigricans in the neck and armpit as a sign of insulin resistance, presence of mycosis in submammary and inguinal folds or epiploic apron fold, or a globular abdomen.
Knee deformity due to osteoarthritis can also be found, very frequently associated with overweight and the presence of peripheral varicopathy with or without associated pigmentary purpuric ocher dermatitis.
Palpation of the liver may give a soft hepatomegaly due to the presence of fatty liver or hepatic steatosis. Other possible findings on abdominal examination are umbilical hernias, diathesis of the rectum, or eventrations in patients with a history of previous abdominal surgery.
Something to keep in mind is the distribution of fat in obesity:
- on thighs in premenopausal women (pear-shaped gynoid obesity)
- in the abdomen in men and in the postmenopausal period (central obesity-android)
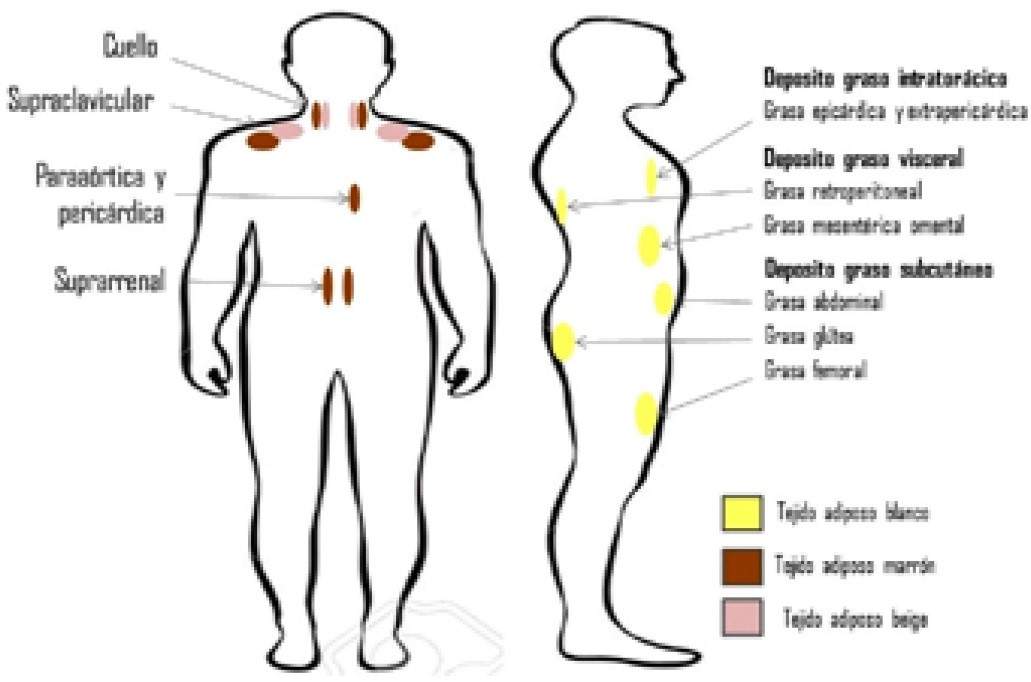
Brown and beige adipose tissue
The composition of adipose tissue includes white adipose tissue, which is the one proposed so far, but also the presence of brown adipose tissue, which has an important role in adaptive thermogenesis since it has a marked thermogenic function, dissipating energy in the form of heat.
This tissue was believed to be present only in the newborn and in children but later its presence was also seen in adults. Unlike white tissue, this tissue presents great innervation and vascularization as well as a significant number of mitochondria and uncoupler protein-1 (UCP-1) that is responsible for the thermogenic function of this tissue.
Recent research has shown that white adipose tissue can, in the face of certain stimuli such as cold and exercise, trans-differentiate into a tissue called beige or pink, which would revert to white tissue when these stimuli disappear or when there is chronic over-intake. [Xii ]
In the next graph we can see the distribution of adipose tissue [xiii]
 This trans-differentiation that would allow an increase in the release of energy as heat may be a hope in the therapy of obesity.
This trans-differentiation that would allow an increase in the release of energy as heat may be a hope in the therapy of obesity.
In conclusion
Obesity is a disease (syndrome) with a number of comorbidities that increase morbidity and mortality in these patients. The distribution of fat is an important factor for this to occur since the deposit of fat at the abdominal level (central obesity) is decisive for the appearance of diabetes, hypertension, dyslipidemia, especially hypertriglyceridemia, hyperuricemia, as well as an increase in some types of cancer. .
Understanding the mechanisms that generate these comorbidities as well as the reasons that lead to excessive intake, violating the intake control circuits, will allow us to get closer to finding a treatment that allows controlling this obesity pandemic.
Working on eating behavior, stimulating physical activity within the possibilities of each patient, intervening in the food industry for the production of healthier products as well as advertising that favors the consumption of extra large portions is a goal to be followed without rest.
As long as you continue to insist on treatments that starve patients instead of seeking changes in eating behavior that are pleasant and thus sustainable in the long term, you will remain a mere observer of a growing problem.
Bibliographic references
[i] Braguinsky.Obesity Knowledge and conflicts.Editorial Acindes 2007
[ii] Wagner Dr et al.Measures of body composition in blacks and whites.A comparative review.Am J Clin Nutr 200;71:1392-402
[iii] Neel JV.Diabetes mellitus.A thrifty genotype rendered detrimental by progress?Am J Human Genet 1962;14:352-362
[iv] Popkin B.The nutrition transition in the developing world differs from past experiences.Public Health Nutrition 2002;5(1ª):205-214
[v] Hales CN, Barker DJP.Type 2(non insulin dependant) diabetes mellitus:the thrifty phenotype hypothesis.Diabetología 1992;35:595-601
[vi] Perinatology and Human Reproduction. Volume 29, Issue 3, July – September 2015, Pages 99-105
[vii] Obesity Wars:Molecular Progress confronts an Expanding Epidemic.Review.Cell Vol 116 . 337-350 January 2004
[viii] Physiopathology of Obesity: Current Perspective. Rev Chil Nutr Vol 44 N ° 3 2017
[ix] Longevity, lipotoxicity and leptin: the adipocyte defense against feasting and famine Roger H. Unger Biochimie oct 2004
[x] Review.The Role of proopiomelanocortin(POMC) neurones in feeding behavior.Nutrition &Metabolism.2007 4:18
[xi] Obesity Keeping hunger at bay M. Schwartz &. Morton. Nature volume 418, pages595–597(2002
[xii] Bartelt A, Heeren J. Adipose tissue browning and metabolic health. Nat Rev Endocrinol 2014; 10(1): 24-36.
[xiii] Physiopathology of obesity: Current perspective Rev. chil. nutr. vol.44 no.3 Santiago 2017