Figueroa Casas Marcelo
The lung fulfills respiratory and non-respiratory functions. Respiratory are related to the exchange of gases between the body and its environment (external respiration).
The non-respiratory functions are very varied, and among them; We can mention: a) synthesis of carbohydrates: mainly mucopolysaccharides, components of bronchial mucus; b) synthesis of phospholipids: from fatty acids from the blood or made in the lung itself, such as dipalmitoyl-lecithin, the main component of the surfactant; c) protein synthesis: useful for the structural support of the lung, such as elastin and the different types of collagen; d) synthesis and release of glycosaminoglycans: heparan sulfate (hevarin), chondroitin sulfate and dermatansulfate; e) synthesis and / or release of vasoactive substances: prostaglandin I2 thromboxane, histamine, slow reacting substance (SRLA), eosinophilic chemotactic factor (ECF-A), kallikrein; f) activation of vasoactive substances: converts to angiotensin I, almost inactive substance, in angiotensin II, the most powerful vasoconstrictor known; g) inactivation of vasoactive substances: bradykinin, serotonin and prostaglandins El, E2 and F2 - alpha by more than 80%, and to a lesser extent histamine and noradrenaline; h) secretion of immunoglobulins: especially IgA, constituting one of the defense mechanisms of the lung; i) platelet production; a large part of platelets are produced by traumatic fragmentation of the cytoplasm of megakaryocytes in the pulmonary microcirculation. constituting one of the defense mechanisms of the lung; i) platelet production; a large part of platelets are produced by traumatic fragmentation of the cytoplasm of megakaryocytes in the pulmonary microcirculation. constituting one of the defense mechanisms of the lung; i) platelet production; a large part of platelets are produced by traumatic fragmentation of the cytoplasm of megakaryocytes in the pulmonary microcirculation.
These functions are of vital importance; This chapter will refer only to respiratory function.
The process of external or pulmonary respiration is carried out through the alveolocapillary membrane, between the alveolar gas from ventilation and the capillary blood from the pulmonary circulation.
Ventilatory function
The contraction of the inspiratory muscles expands the rib cage, lowering intrapleural and intraalveolar pressure, allowing air to enter the lungs. When inspiration ends, the muscles relax, there is a passive return due to the elastic retraction of the lungs that increases the alveolar pressure above atmospheric pressure, and expiration occurs that reaches the resting situation, just where they balance. the elastic retraction forces of the lung that tend to collapse and those of the rib cage that tend to expand.
The ventilatory capacity depends on the resistance of the airway, the volume and the lung elasticity; of muscular strength; of ventilatory control by the nervous system and of an adequate distribution of ventilation in the different alveolar units.
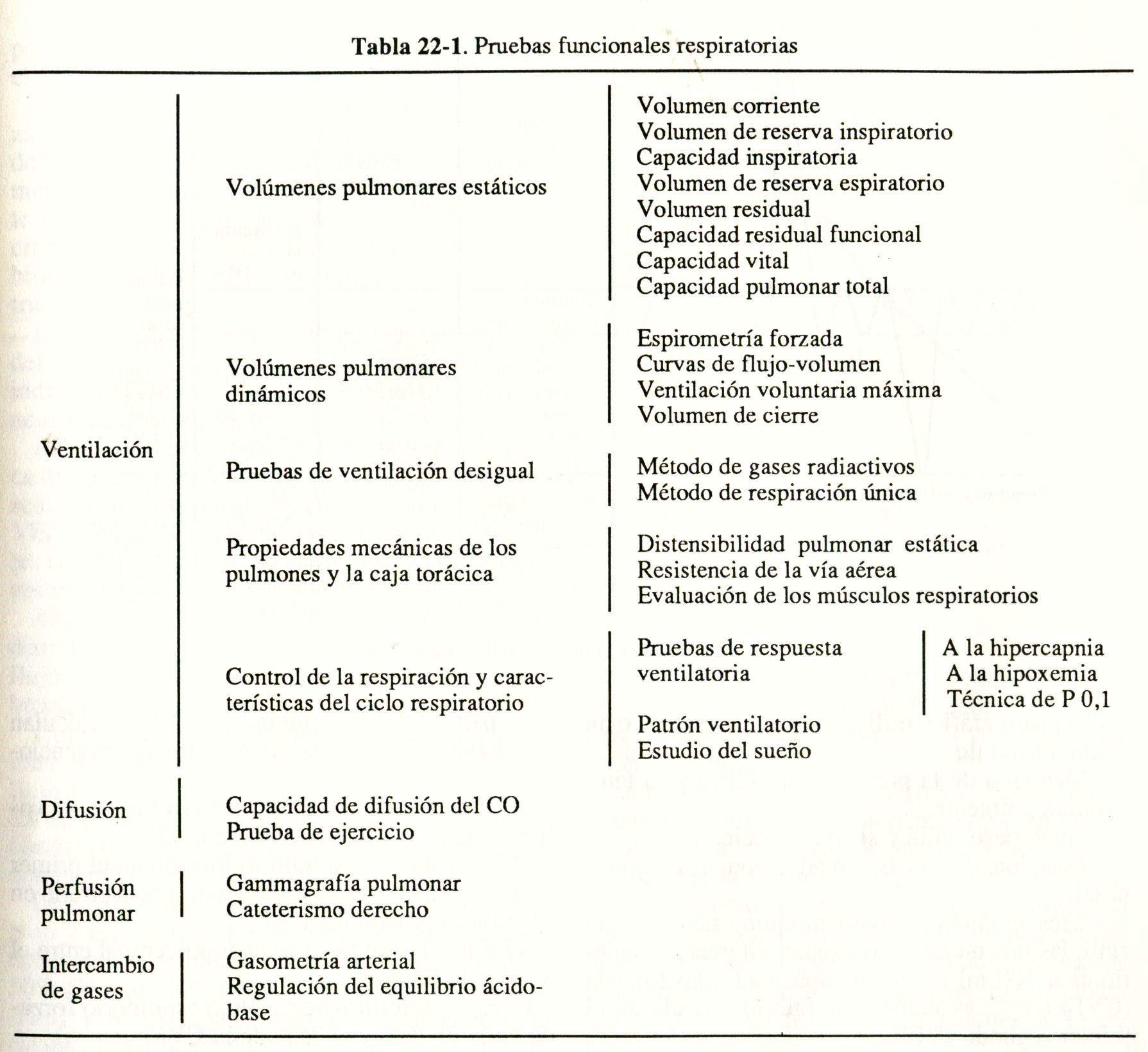
To study each of these determining factors of ventilatory function, there are different tests, as can be seen in Table 22-1.
Diffusion
The gases that reach the alveoli cross the alveolocapillary membrane by simple passive diffusion and follow Fick's law; this diffusion is directly proportional to the surface of the membrane and to the difference in gas concentration on both sides (alveolus and capillary), and inversely proportional to the thickness of the membrane. The rate of gas exchange depends directly on the solubility of the gas and is inversely proportional to the square root of its molecular weight.
O2 and CO2 have almost the same molecular hair, but CO2 is much more soluble and diffuses 20 times faster than 02.
Under normal conditions, the O2 and CO2 pressures in the alveolus and in the pillar blood equilibrate in 0.25 second with 0.75 second in contact (Fig. 22-1)
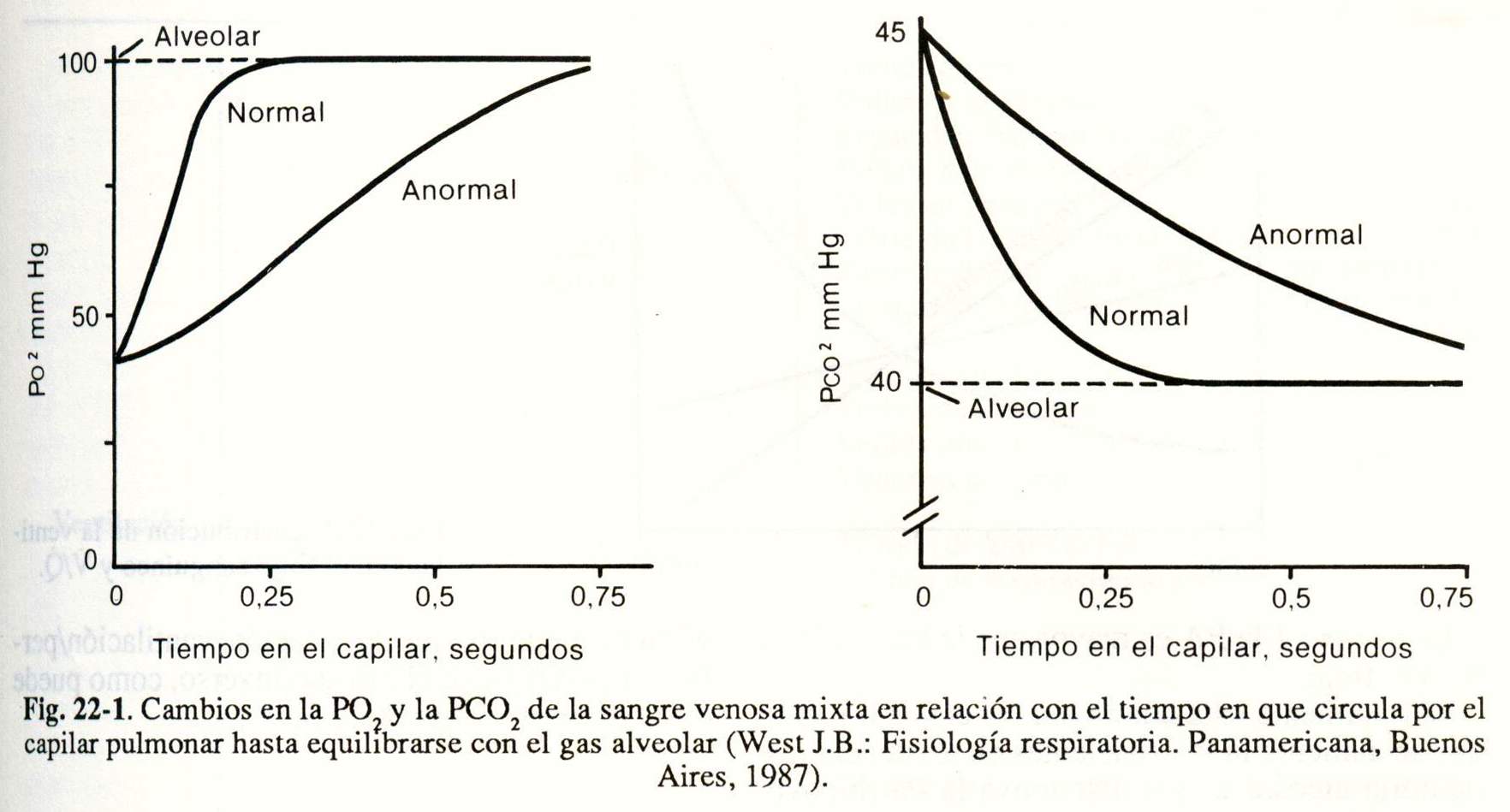
Resistance to O2 diffusion is determined by the alveolocapillary membrane and by the reaction that causes oxyhemoglobin within the erythrocyte.
Clinically, CO (carbon monoxide) is generally used to investigate diffusion disorders.
Functional pulmonary circulation
The pulmonary circulation is a low-pressure system through which the entire cardiac minute volume passes and in which significant increases in blood flow can occur without substantial changes in pressures; This is due to the opening of numerous vessels that under normal conditions are collapsed (recruitment phenomenon) and the fact that the arterioles have little smooth muscle, which favors an increase in their caliber (distension phenomenon).
The distribution of blood flow is uneven due mainly to the effect of gravity: the capillaries at the lung bases receive more flow than those at the vertex.
West developed a blood flow model by dividing the lung into zones, based on the relationship between pulmonary arterial pressure (Pa), alveolar pressure (PA), and pulmonary venous pressure (Pv), and to which he later added interstitial pressure ( Pi) (Fig. 22-2).
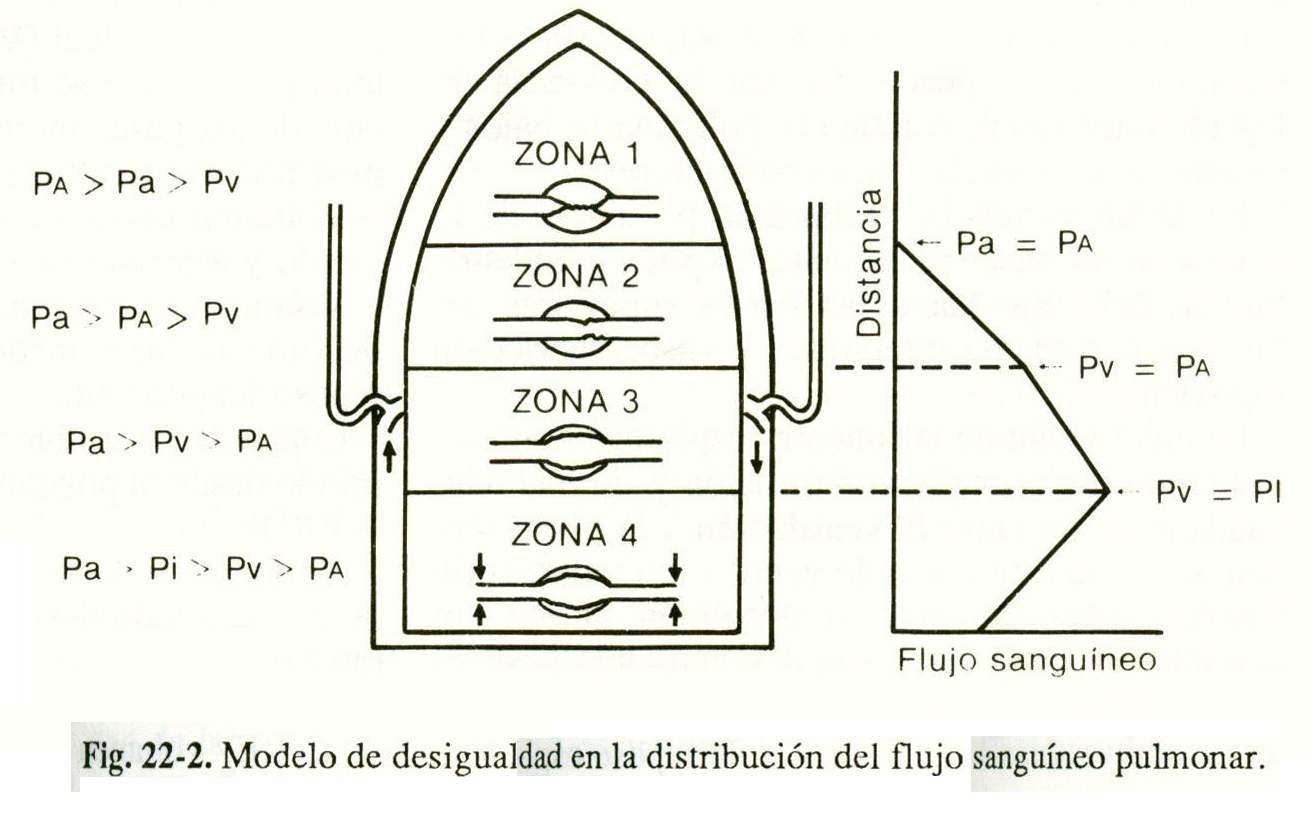
In zone 1 the PA is greater than the Pa and Pv and there is no flow.
Normally this condition does not exist unless the BP is increased (patients on mechanical ventilation) and / or the Pa is decreased (hypovolemia, vasodilator drugs).
In zone 2 the Pa is greater than the PA and this, in turn, is greater than the Pv, for which the flow is determined by the difference between the Pa and the PA.
In zone 3 the Pa exceeds the Pv and this is higher than the PA, the flow being dependent on the difference between the Pa and the Pv, as in the systemic circulation.
In zone 4 Pi is greater than Pv and the flow depends on the gradient between Pa and Pi.
Pi is the result of two opposing forces acting on the extraalveolar vessels:
a) Tension of the vessel wall: it is determined by muscle tone. It increases during acidosis, hypercapnia, due to neurotransmitters and vasoactive hormones, and due to the decrease in alveolar PO (hypoxic vasoconstriction).
b) Perivascular pressure: the small vessels are kept open by the traction of the parenchyma on the conjunctival sheaths that surround them.
When the lung is inflated, the perivascular pressure is more negative and the vessels are more distended.
Pi affects flow when it is higher than Pv, a situation that can occur due to the presence of interstitial fluid, low lung volumes and substances, or vasoconstrictor stimuli.
In heart failure. the presence of zone 4 in the lung bases explains the redistribution of flow towards the upper parts of the lung by interstitial edema and hypoxic vasoconstriction.
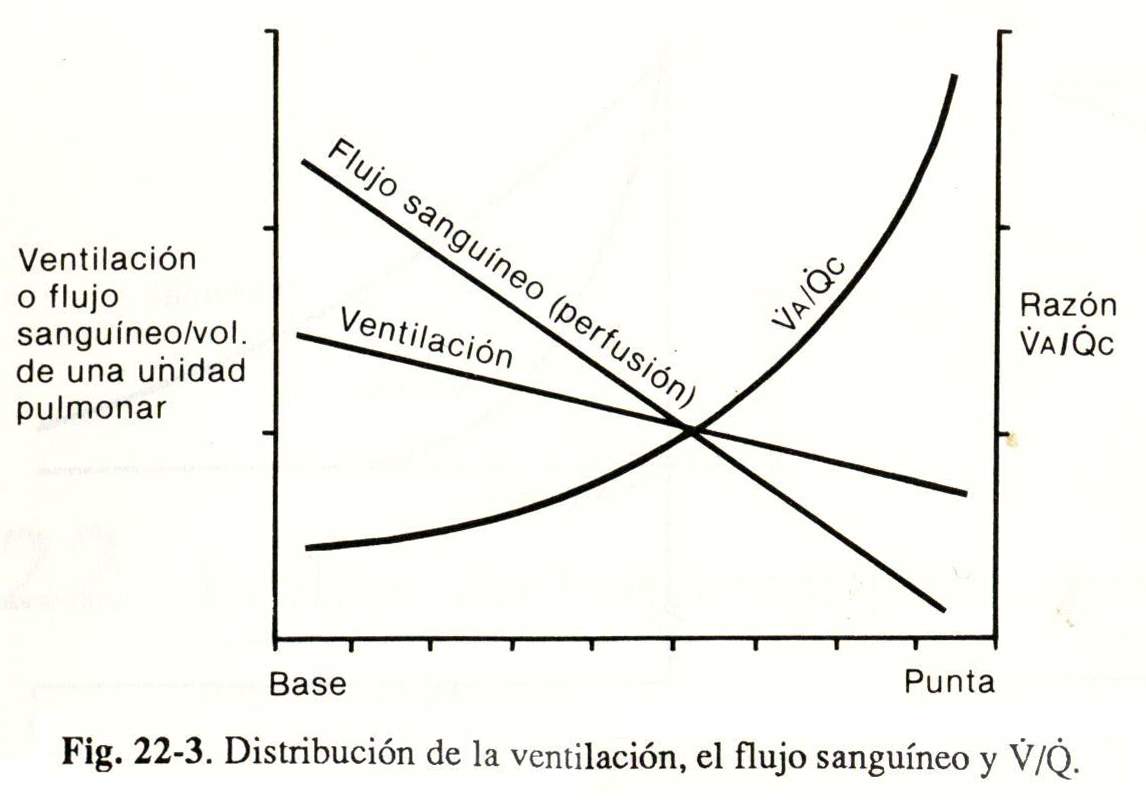
The effectiveness of pulmonary respiratory function requires good diffusion and an adequate relationship between ventilation and perfusion. Despite the difference in ventilation and perfusion that normally exists in the lung, both are maximum at the bases and descend to the apex, while the ventilation / perfusion (V / Q) ratio follows the reverse path, as can be seen in Figure 22-3.
Tests for examination of respiratory function
There is a wide variety of tests (Table 22-1) to assess pulmonary respiratory function; some are very simple and widespread, others more complex and used only in special cases, and the rest restricted to research protocols.
Ventilation
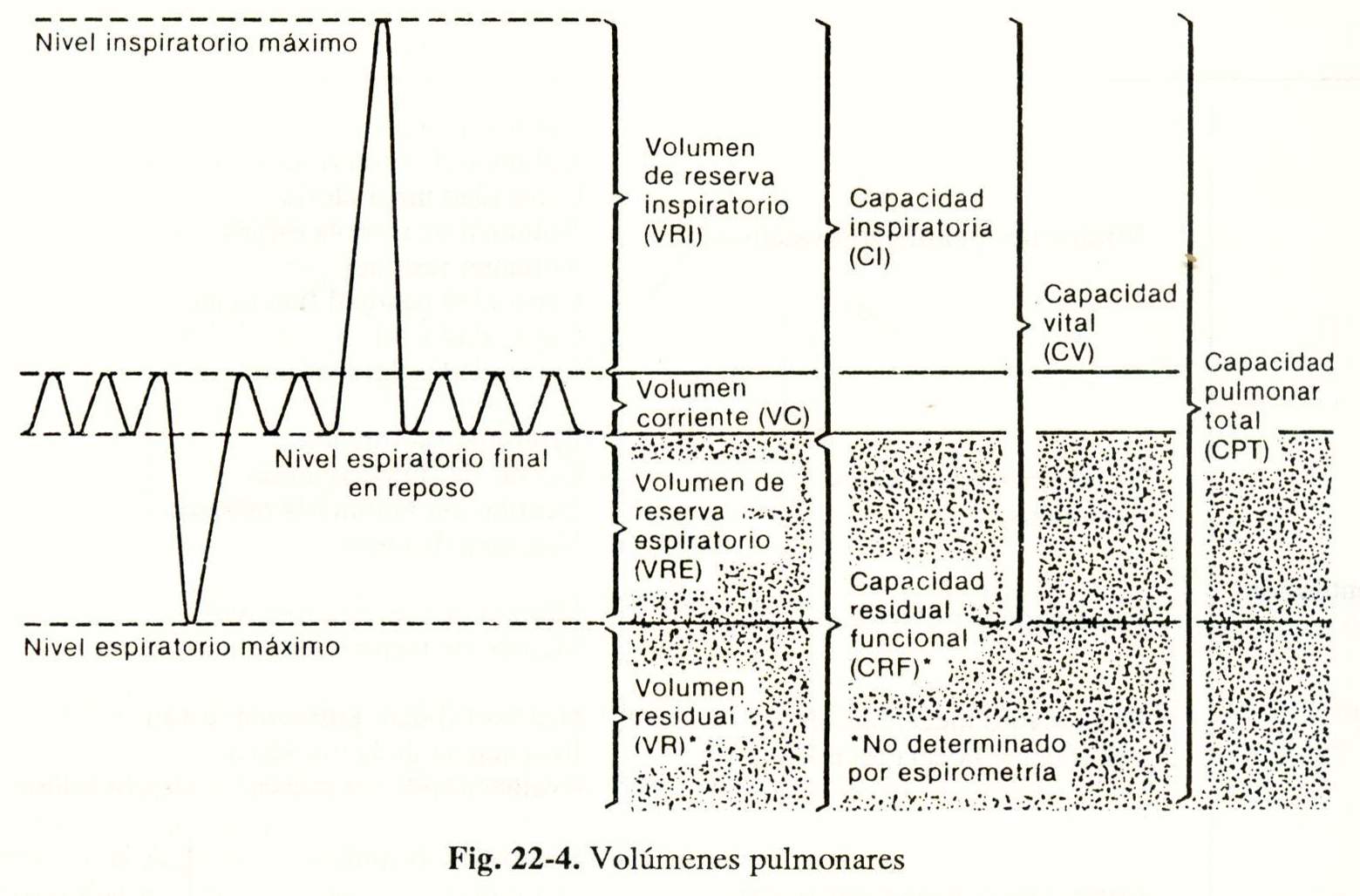
Static lung volumes
The measurement of lung volume in different positions of the rib cage, from maximum inspiration to maximum expiration, reflects the elastic properties of the respiratory system (expansion and / or reduction capacity of the lung and the cage).
All measurements are made with a spirometer (Fig. 22-4), except for residual capacity. functional function (CRF) and those derived from it, residual volume (VR) and total lung capacity (CPT), which are measured by the inert gas dilution method (He, Ne, N2), and body plethysmography total.
Tidal volume (Ve.): Inspired and expired air volume in a normal breath.
Inspiratory Reserve Volume (IRV): maximum volume of air inspired from the inspiratory rest position.
Inspiratory capacity (IC): volume of air inspired from the expiratory rest position (VC + VRI).
Expiratory Reserve Volume (ERV): volume of air expired from the expiratory rest position.
Residual volume (RV): volume of air that remains in the lungs after a forced expiration.
Functional residual capacity (FRC): volume of air that remains in the lungs from the position of expiratory rest (VRE + VR).
Vital capacity (CV): maximum volume of air that can be exhaled after maximum inspiration.
Total lung capacity (TPC): volume of air that the lung contains at the end of a maximum inspiration.
Usefulness of the measurement of static lung volumes. The decrease in volumes and especially in CRF and VR suggests the presence of a restriction that may be caused by a reduction in the compliance of the lungs (with the consequent rigidity and increased elastic recoil, tending to a volume of rest smaller as occurs in diffuse interstitial fibrosis) or by decreased compliance of the rib cage, as in kyphoscoliosis.
Increased volumes indicate pulmonary hyperinflation due to airway obstruction; examples are emphysema, chronic bronchitis, and asthma attacks.
Dynamic lung volumes
The air volumes displaced during inspiration or expiration make up the dynamic lung volumes and are assessed by measuring the flow or velocity of the inspired or expired air using forced spirometry, flow-volume curves, maximum voluntary ventilation, and volume closure.
Forced spirometry (EF). It is the simplest test and one of the best for the amount of data it provides, the ease of its execution and the low cost.
The EF is performed after a maximum inspiration, obtaining a spirogram in which the volume exhaled during a forced, fast, complete expiration and the time elapsed are recorded.
EF technique. The following should be taken into account:
- Graphic recording using a spirometer or pneumotachograph.
- Measurement of atmospheric pressure and ambient temperature.
- Age, weight, height and sex of the patient.
- Standing or sitting position, with or without nose clip.
- At least three maneuvers, provided that between the best two there are no differences greater than 100 ml or 5% in forced vital capacity (FVC »or forced expiratory volume in the first second (FEV)
- The values obtained are correlated with the estimated by the prediction equations of EF (average value of each parameter in healthy people of the same sex, age, height and weight), and are expressed as a percentage of normal.
From the spirogram (Fig. 22-5), the different conventional spirometric parameters are calculated:
CVF; Forced vital capacity (in ml): is the volume of air exhaled during PE.
FEV1; Forced expiratory volume in the first second (in ml): it is the volume of expired air, in the first second of the PE.
VEF / FVC; (in%): percentage ratio between FEV1 and FVC.
FEF 25-75% (in liters / sec): forced expiratory flow between 25% and 75% of the FVC.
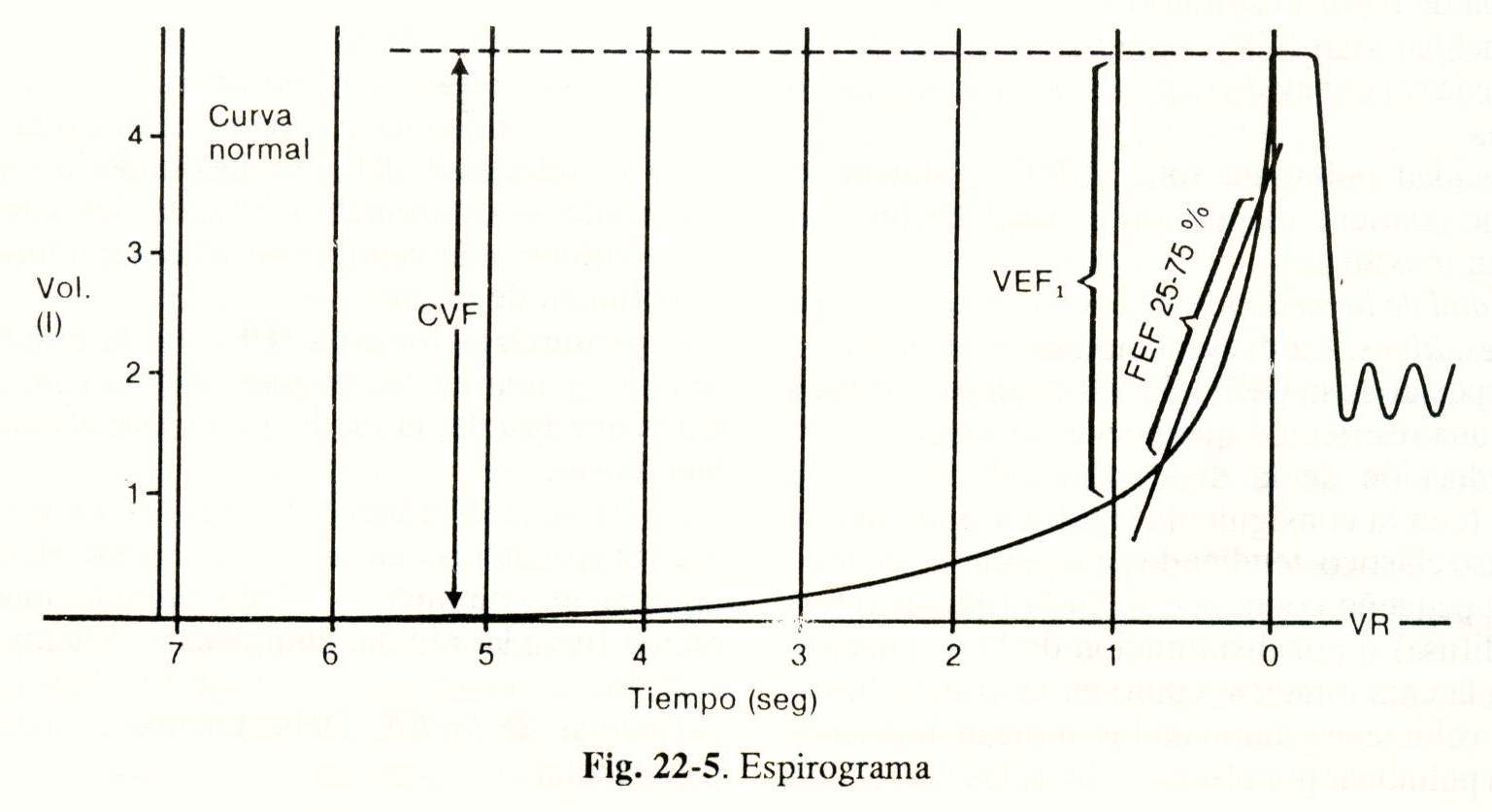
Clinical interpretation of PE. After doing the spirogram and calculating the basic parameters, it is possible to find the following patterns: normal, obstructive, restrictive, and mixed.
Normal pattern: the lower limit of normal for FVC and FEV is 80% of theoretical and for FEF 25-75% 60% of theoretical.
Obstructive ventilatory alteration: characterized by a decrease in FEV1, FEV / FVC and FEF 25-75%, with a normal or moderately decreased FVC. This pattern may be present in patients with emphysema, asthma, and chronic bronchitis. In addition, the bronchodilator test (PBD) is performed from the PE to determine if the airway obstruction is fixed or reversible.
PBD is positive when it produces an increase in FEV1 and FVC by at least 25%, indicating the reversibility of the obstruction as it usually occurs in asthma.
Restrictive ventilatory alteration: there is a clear decrease in FVC with reduced or normal FEV1 and FEF 25-75%, while the FEV1 / FVC ratio is normal. This pattern is seen in patients with pulmonary fibrosis, kyphoscoliosis, obesity, neuromuscular diseases, and others.
Mixed ventilatory alterations: there is a decrease in FVC and signs of airflow obstruction. Granulomatous diseases, bronchiectasis, and others have this pattern.
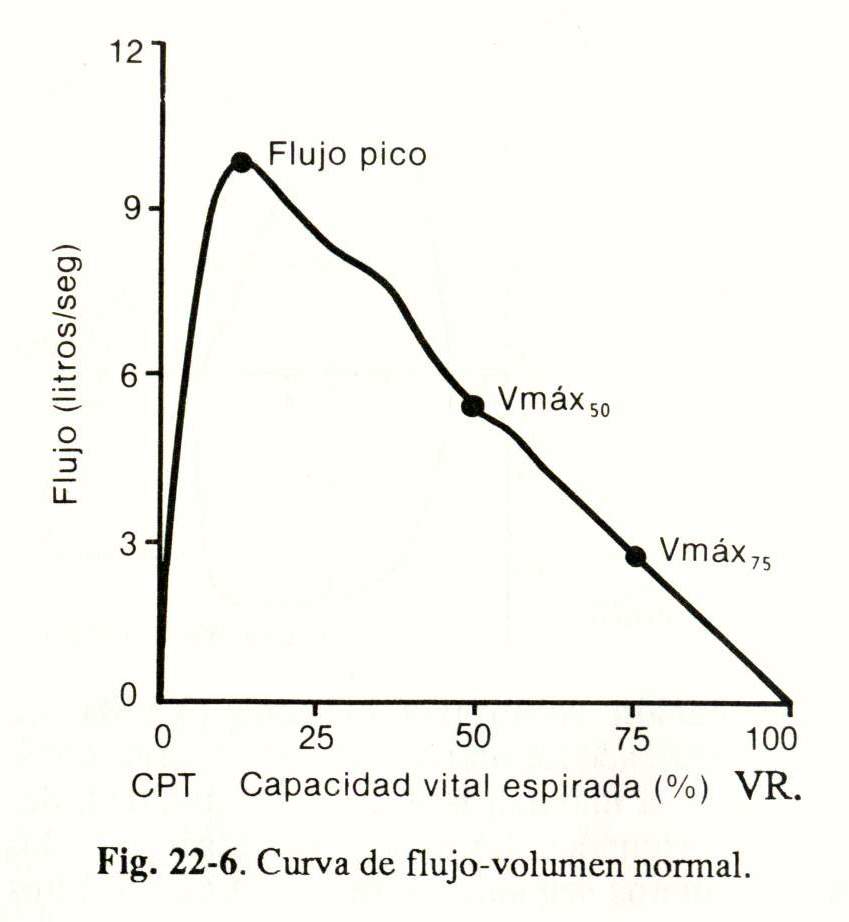
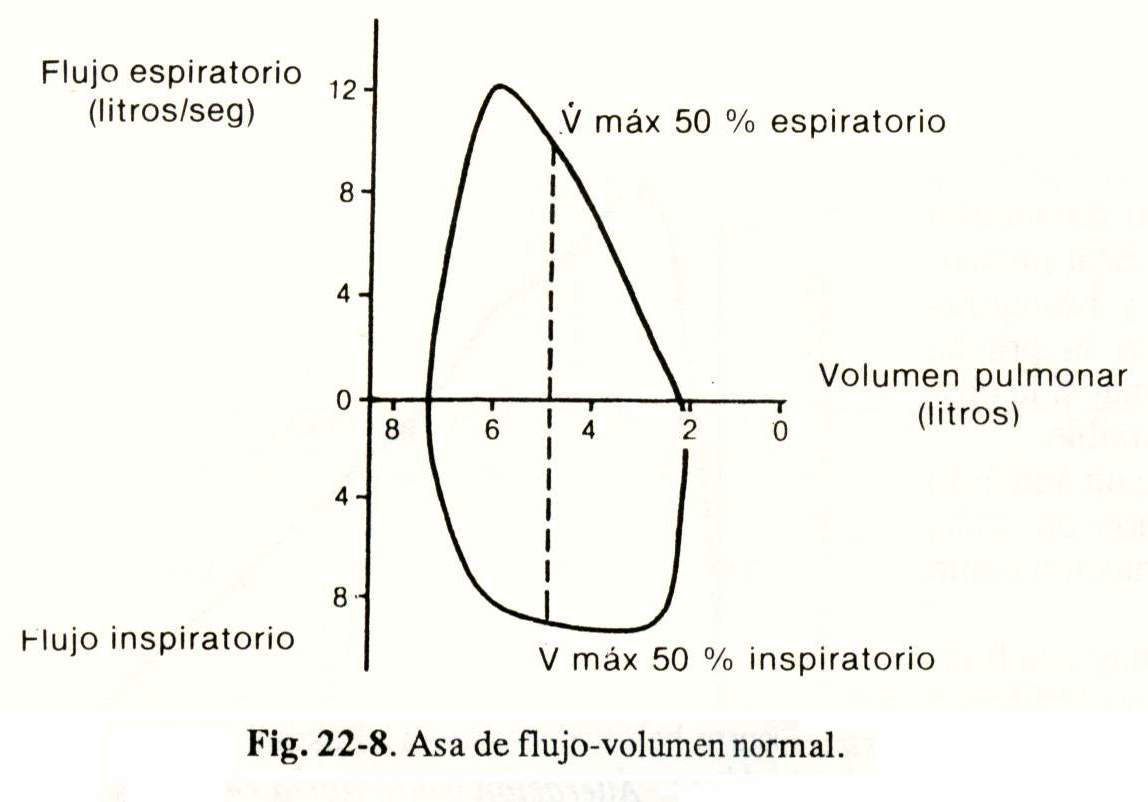
Flow-volume curves. During a maximal expiratory maneuver, flow velocity is recorded in relation to lung volume (Fig. 22-6), starting from the CPT. Flow is maximum at the beginning of expiration and then decreases linearly until reaching VR.
Once the record is made, the peak flow and maximum flow rates are calculated for a given expired volume, generally at 50% (V max. 50%) or at 75% (V max. 75%) (Fig. 22- 6) And they are expressed as a percentage of the established value according to age, sex and body surface area.
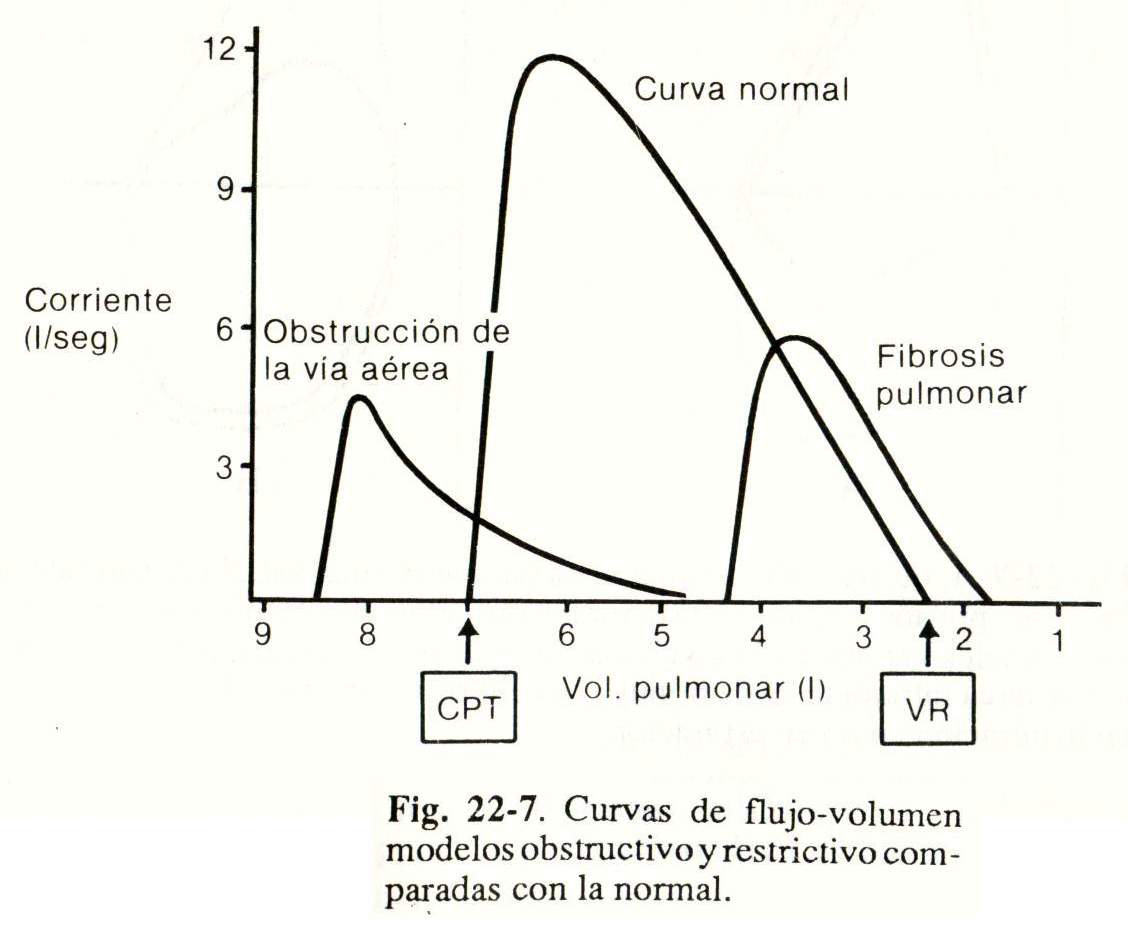
Interpretation of the flow-volume curve. Obstructive and restrictive models compared to normal are shown in Figure 22-7.
In obstructive pulmonary diseases (chronic bronchitis, emphysema), expiration begins and ends with abnormally high volumes and the flow rate is much lower than normal. Flow rates V max. 50% and V max. 75% are diminished.
In restrictive diseases (interstitial fibrosis), lung volumes are greatly reduced, but the flow velocity is greater than normal when related to lung volume.
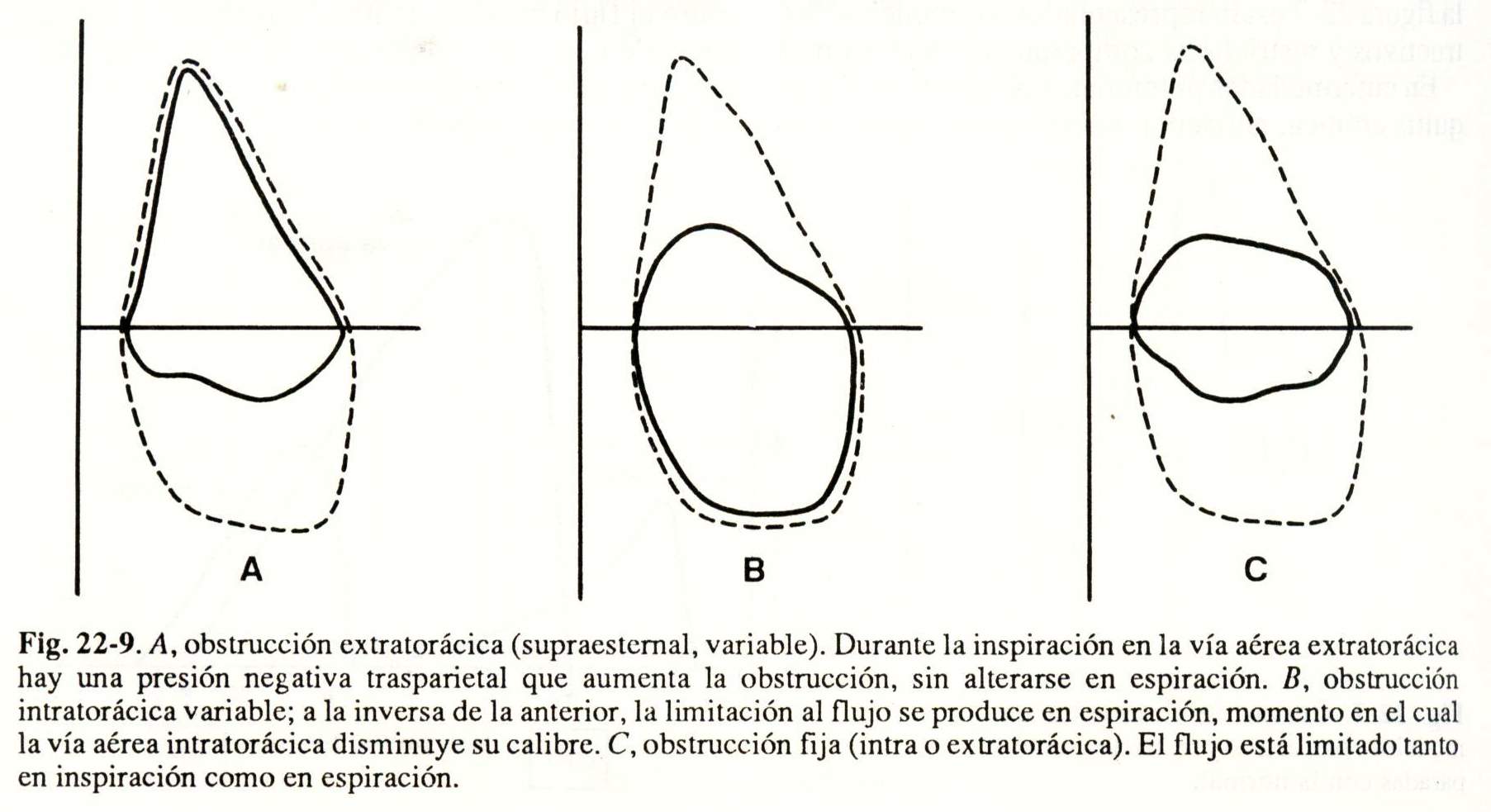
If the flow and volume recording during forced expiration is completed with a maximal inspiration maneuver, a flow-volume loop is obtained (Fig. 22-8), which is used for the diagnosis and localization of obstructions in the airway . higher.
The interpretation is made taking into account the morphology of the curve (Fig. 22-9) and the ratio between the maximum flow at 50% inspiratory and expiratory (Vmax, 50% inspiratory / Vmax. 50% expiratory), which normally it must be close to 1, but always greater than unity.
 Maximum Voluntary Ventilation (VVM). It is done by making the patient breathe steadily, with maximum speed and depth, for 15 seconds. Ventilation is measured in the first twelve seconds and is expressed in liters per minute.
Maximum Voluntary Ventilation (VVM). It is done by making the patient breathe steadily, with maximum speed and depth, for 15 seconds. Ventilation is measured in the first twelve seconds and is expressed in liters per minute.
VVM has a good correlation with FEV1, accepting that: VVM (1 / minute) = FEV1 (liters) x 35.
This test is influenced by the resistance of the airway and the function of the respiratory muscles.
MVV is difficult to measure, strenuous for critically ill patients, and correlates with FEV1, which is why its application has decreased. It would be reserved for the preoperative evaluation of lung resections due to its predictive value of postoperative complications.
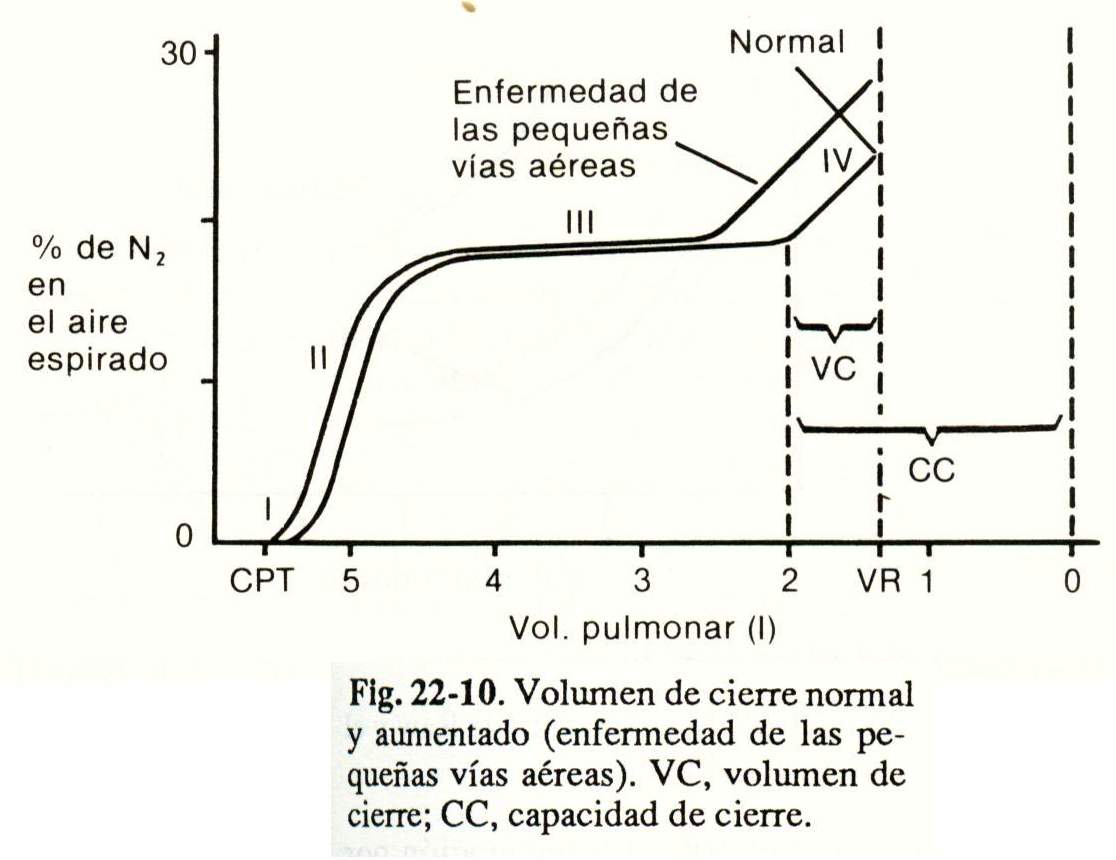
Closing volume. The closure volume theoretically measures the point at which the small airways of the lung bases close. It is calculated using a N2 concentration meter in exhaled air after a single and maximum inspiration with 100% O2.
When inspiration begins, the air that is in the upper airways, rich in N2, enters the alveoli of the upper areas of the lung while 100% O2 goes preferentially to the basal portions, for which the N. In the alveoli of the bases will be much lower than that of the vertices.
By recording the concentration of N2 in expired air as a function of lung volume, a graph is obtained (Fig. 22-10) in which four phases are described:
Phase I - Contains only O2 that remained in dead space.
Phase II: rapid increase in the concentration of N2, due to the mixture of alveolar gas and the airways.
Phase III: plateau, corresponds to the emptying of the alveoli of different regions.
 Phase IV: there is a rapid increase in the concentration of N2 that comes from the alveoli of the upper areas of the lung due to the closure of the small airways of the bases.
Phase IV: there is a rapid increase in the concentration of N2 that comes from the alveoli of the upper areas of the lung due to the closure of the small airways of the bases.
The volume of air exhaled from the junction point of phases III and IV is the closing volume that is expressed as a percentage of the Cv. In young and normal people, the closure volume is approximately 10% of the CV.
 If the VR is known, the closing volume can also be expressed as the closing capacity (in liters), which is equal to the sum of the closing volume and the VR.
If the VR is known, the closing volume can also be expressed as the closing capacity (in liters), which is equal to the sum of the closing volume and the VR.
The volume and closing capacity increase with age and in emphysema, asthma, and bronchitis. chronicle.
 Uneven ventilation tests
Uneven ventilation tests
The radioactive gas method and the breathing method will be described. only.
Radioactive gas method. The patient inhales Xe 133 whose radiation is captured by counters placed outside the thorax, recording the distribution of the inspired xenon in the different regions.
In normal people in an upright position, ventilation is maximum at the bases. pulmonary, decreasing towards the vertices. In dorsal decubitus, ventilation is greater in the posterior areas and in lateral decubitus the lung that is below ventilates better.
Single breath method. It is performed with 100% oxygen, measuring the expired N2 concentration as described in the closing volume with its four phases.
The plateau phase III reflects the uniform dilution of alveolar N2 and inspired 02. When in phase III the concentration of expired N2 continues to increase (there is no plateau), it means that there is an uneven dilution of the alveolar N2 by the inspired 02, showing uneven ventilation.
The single breath method is the simplest, fastest and safest method to measure the degree of uneven ventilation of the lung. It is increased in the majority of obstructive pulmonary diseases and in some of the restrictive type.
 Mechanical properties of the lungs and rib cage
Mechanical properties of the lungs and rib cage
Of the mechanical properties of the lung and the rib cage, the most important ones for understanding clinical alterations will be analyzed: lung compliance, airway resistance and the effectiveness of the respiratory muscles to mobilize the rib cage.
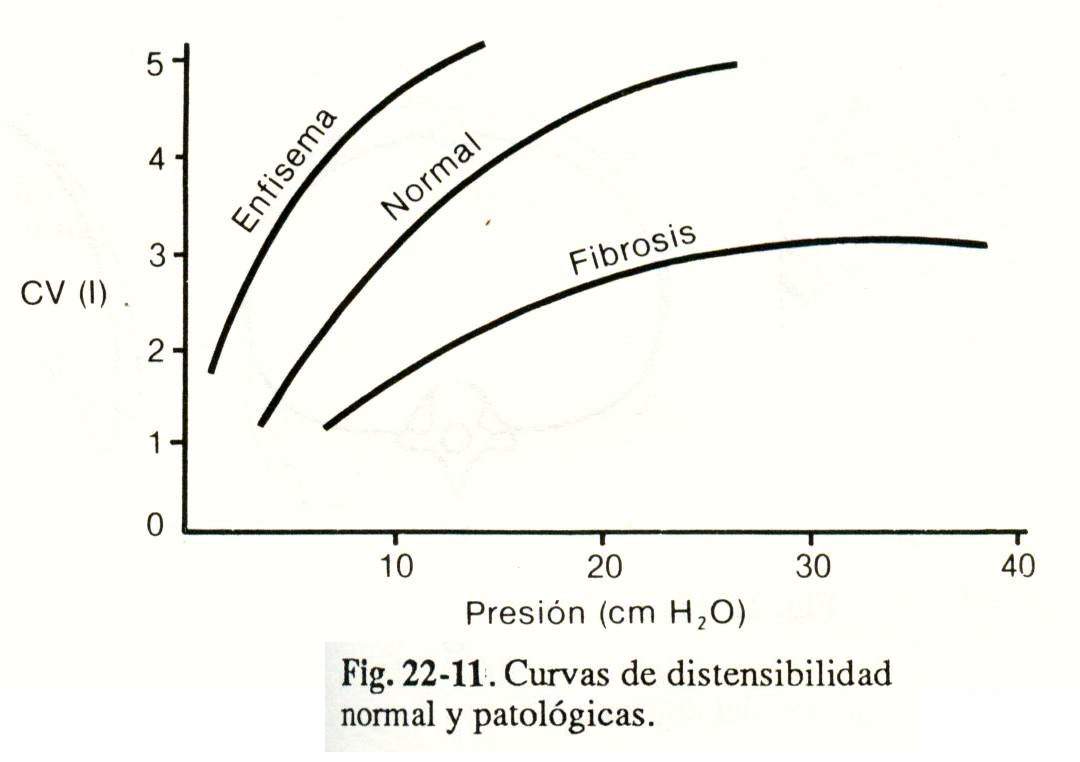
Static lung compliance. It is expressed from the relationship between the changes in lung volume produced by a certain variation in transpulmonary pressure (alveolar pressure-pleural pressure).
It is determined when the airflow is null and the glottis is open, which is the state in which the alveolar pressure is equal to the atmospheric one (that is = cm H2O); therefore, the transpulmonary pressure is referred only to the pleural pressure.
Method. The patient takes inspirations at different lung volumes (measured with spirometers or pneumotachograph); At the end of each inspiration, he maintains an apnea for at least 3 seconds with the glottis open, at which time pleural pressure is recorded through a balloon catheter placed in the esophagus (Fig. 22-11).
Interpretation. Normal lung compliance is 200 ml / cm H2O. Static compliance is decreased in pulmonary fibrosis and increased in emphysema (Fig. 22-11).
Airway resistance (Raw). Raw is influenced by lung volume, elastic recoil, and airway geometry.
During oral expiration, the mouth, pharynx, larynx and glottis represent 50% of the Raw, the trachea and bronchi larger than 20mm 40% and the small airway 10%. Breathing through the nose is double or triple the whole of the Raw.
The Raw is calculated from the quotient between the alveolobucal pressure difference and the air flow.
Raw = alveolar pressure - mouth pressure
Air flow.
Alveolar pressure is measured by body plethysmography and air flow with a pneumotachograph. The relationship between Raw and lung volume is depicted in Figure 22-12.
Interpretation. Raw is increased in obstructive diseases and decreased or close to the lower limit of the normal range in restrictive diseases (Fig. 22-12).
To assess Raw in the clinic, forced spirometry and flow-volume curves are usually used.
Assessment of respiratory muscles. The respiratory muscles are the effectors of the respiratory control system.
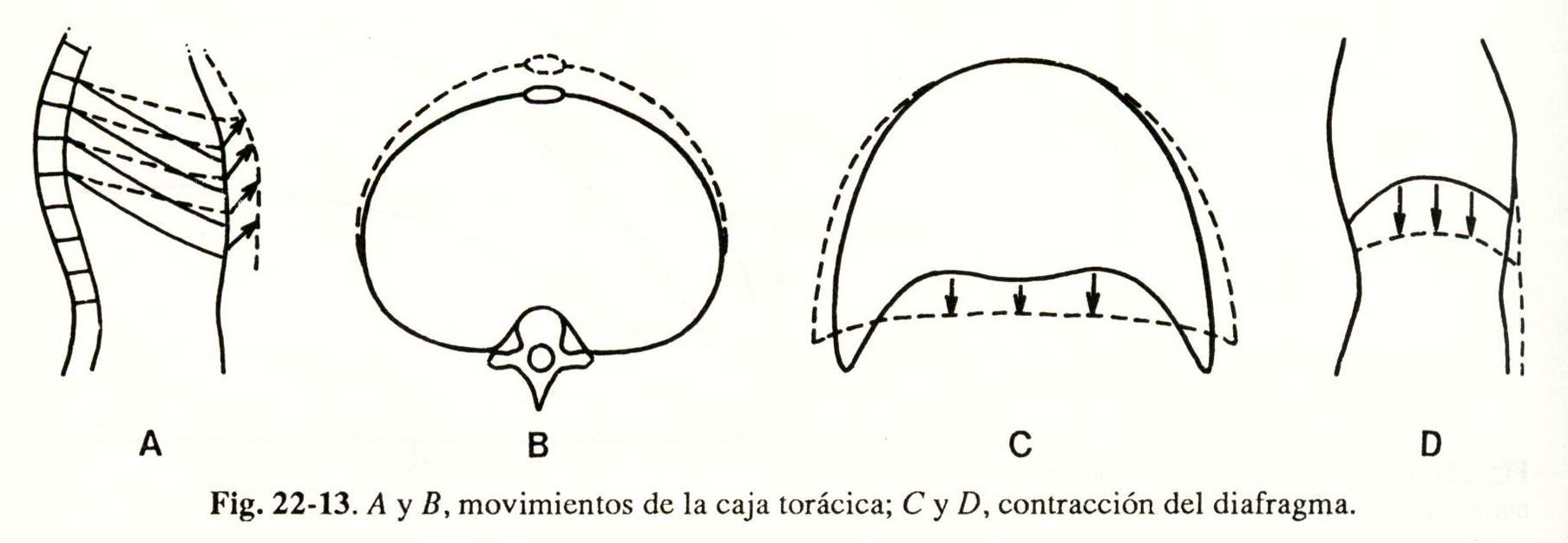
On inspiration, the thoracic cage increases its anteroposterior and transverse diameters (Fig. 22-13, A and B) due to the action of the external intercostal muscles (and on some occasions by the accessories, scalenes and sternocleidomastoids) and of the diaphragm, the main inspiratory muscle , which moves the abdominal content down and forward and lifts. the rib margins (Fig. 22-13, C and D).
Muscle evaluation. It includes clinical, radiological, electromyographic data and tests. functional.
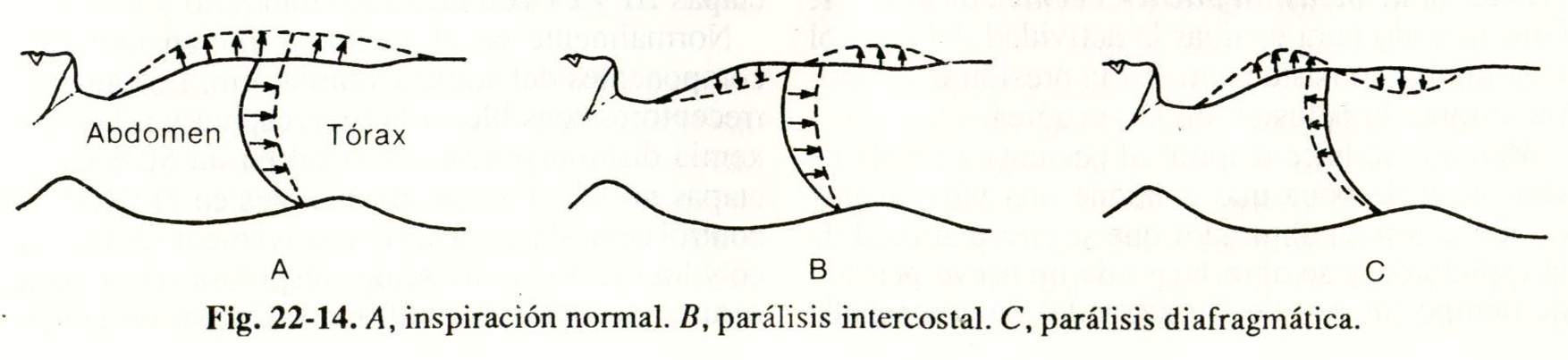
 Clinical evaluation. It is performed by observing the patient in the supine position from the side. On inspiration the thorax and abdomen should expand (Fig. 22-14, A). If the thorax tends to depress there is weakness. or paralysis of the intercostal muscles (Fig. 22-14, B). If the abdomen becomes depressed, there is paralysis or diaphragmatic paralysis (Fig. 22-14, C). Sometimes abnormal movements are better detected. placing one hand on the thorax and the other on the abdomen.
Clinical evaluation. It is performed by observing the patient in the supine position from the side. On inspiration the thorax and abdomen should expand (Fig. 22-14, A). If the thorax tends to depress there is weakness. or paralysis of the intercostal muscles (Fig. 22-14, B). If the abdomen becomes depressed, there is paralysis or diaphragmatic paralysis (Fig. 22-14, C). Sometimes abnormal movements are better detected. placing one hand on the thorax and the other on the abdomen.
Radiological evaluation. It is important for the diagnosis of paralysis of a hemidiaphragm, which will be raised over the one that normally contracts. When diaphragmatic paralysis is complete, fluoroscopic examination is better, where it will be observed that on inspiration the diaphragm rises instead of moving downwards (paradoxical movement).
Electromyographic evaluation.
Electromyography is used to explore. conduction velocity after stimulation of the phrenic nerve and electrical activity generated by muscle contraction. by means of intraesophageal electrodes, needle electrodes inserted into the diaphragm through the 6th or 7th intercostal space. or by surface electrodes in the same location.
Functional testing. In forced spirometry, a fall in forced vital capacity greater than 30% when going from the upright position to the supine position suggests diaphragmatic paralysis (in the upright position, the paradoxical movement of the diaphragm decreases due to the traction exerted on it by the abdominal viscera) .
The maximum forces they develop. respiratory muscles are determined. by the maximum inspiratory and expiratory pressures (Pi max and Pe max), which are measured through a mouthpiece that allows static efforts to be made by interrupting airflow at any lung volume; but usually the Pi max is registered after a complete expiration (inspiratory effort from RV) and the Pe max after a complete inspiration. (expiratory effort from CPT).
The forces generated by the diaphragm are determined by the transdiaphragmatic pressure (Pdi), which is calculated from the difference between abdominal pressure and pleural pressure:
Pdi = P abdominal - P pleural
Method. A balloon catheter is placed in the stomach to measure abdominal P and another in the middle third of the esophagus to record pleural P. While the patient breathes at tidal volume, the difference between the two pressures is the Pdi, and when he makes a maximum inspiratory effort, without air flow and from the CRF or RV, it is the Pdi max. Subsequently, the quotient Pdi / pdi max is calculated, whose normal value is less than 0.4.
The development of respiratory muscle fatigue depends on the force (pdi / PdL max) and the time that inspiratory muscle contraction (Ti) lasts over the total duration of the respiratory cycle (Ttot). The normal Ti / Ttot is 0.38 or less. From these two relationships, the tension x time index (TTdi) is obtained, which defines the threshold for respiratory muscle fatigue (it must not exceed 0.15):
TTdi = (pdi / Pdi max X Ti / Ttot)
The critical TTdi can be achieved by any combination of Pdi / Pdi max and Ti / Ttot.
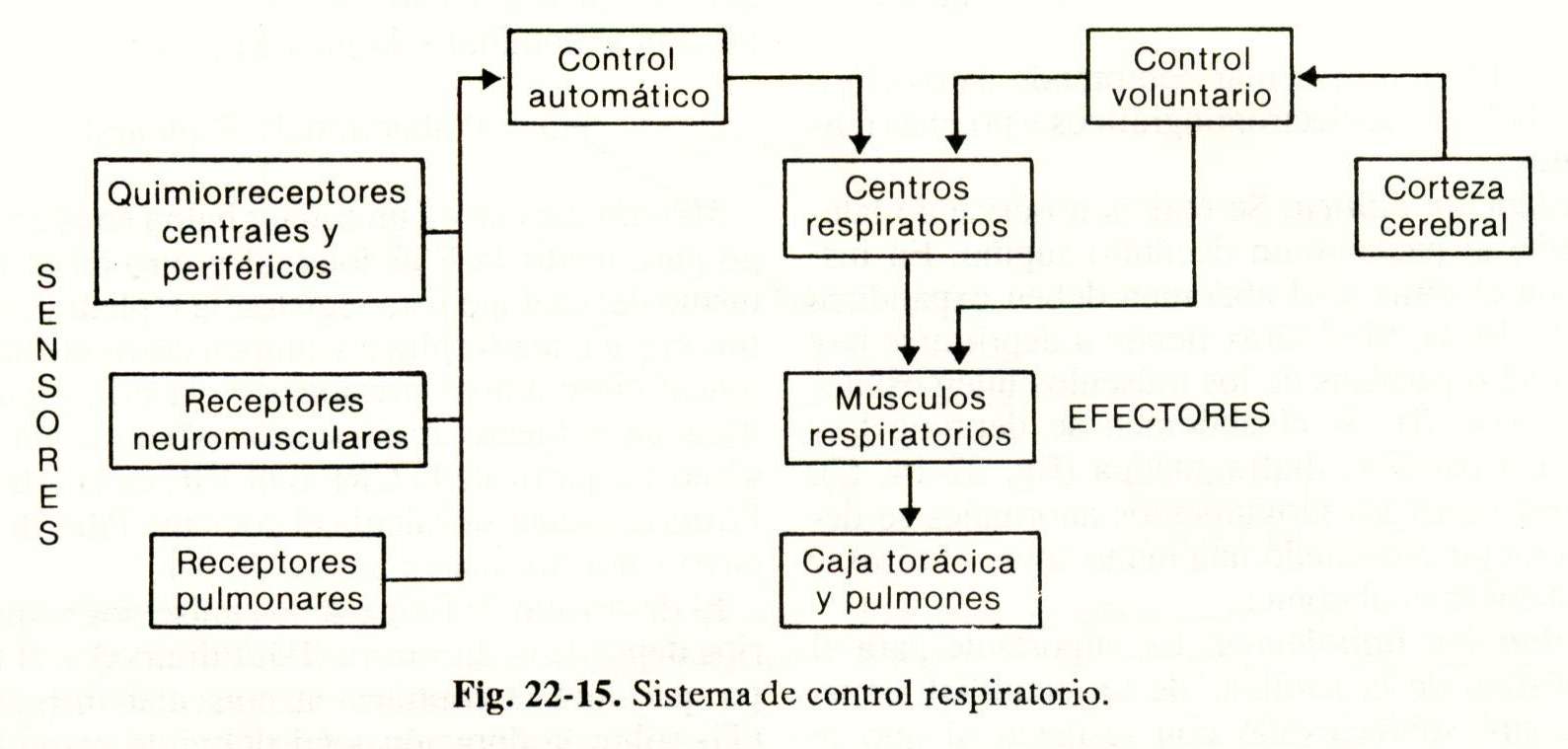
Control of respiration and characteristics of the respiratory cycle
The regulation of ventilation is done through the CNS: the cortex. The brain is in voluntary control and the brain stem is in automatic control.
Figure 22-15 outlines the respiratory control system, which consists of three critical components:
1) Sensors: receive information and transmit it to the central control.
2) Central brain control: it processes the information and sends impulses to the effectors.
3) Effectors: they are the respiratory muscles.
Ventilatory response tests. The two best studied ventilation stimuli are hypercapnia and hypoxemia.
Ventilatory response to hypercapnia. The increase in PCO2 is perceived by a central chemoreceptor located in the bulb. Typically, for every mm Hg increase in PC02, ventilation increases by 2 to 5 liters / minute.
 Method. A bag is filled with a 7% CO2 / oxygen mixture by having the patient breathe in and re-inhale from the bag for a few minutes. The CO2 in the bag increases and the increase in ventilation is determined for each mm Hg increase in PCO2.
Method. A bag is filled with a 7% CO2 / oxygen mixture by having the patient breathe in and re-inhale from the bag for a few minutes. The CO2 in the bag increases and the increase in ventilation is determined for each mm Hg increase in PCO2.
When the CO concentration in the bag is 15%, ventilation reaches its maximum, approximately 100 liters / minute.
The answer. Ventilation to hypercapnia decreases during sleep, the administration of sedatives or anesthetics, genetic factors, age and when there is a chronic increase in PaCO2.
The decrease in blood pH, regardless of PaCO2, also stimulates ventilation.
Ventilatory response to hypoxemia. The decrease in PaO is detected by peripheral chemoreceptors (carotid and aortic) but the response increases. Ventilation is irrelevant if the PAO2 does not fall below 60 mm Hg. Larger drops cause large increases in ventilation.
Method. The patient breathes from a bag containing 24% O2 AND 7% CO2. On rebreathing, the inspired O2 decreases to 40 mm Hg (keeping the PCO2 constant through a CO2 absorption system), while the response is quantified. ventilatory.
The answer. Ventilation to hypoxemia is decreased in extreme obesity, in those who receive depressant drugs: or opiates and with age.
Buccal occlusion pressure - Technique of P 0.1.
Another method of evaluating respiratory control activity is to measure inspiratory pressure during airway occlusion.
Method. The patient is made to breathe through a mouthpiece that contains an inspiratory valve with an obturator that closes at the end of expiration and opens after a short period of time, (less than 1/2 second) after the start of expiration. inspiration. The negative pressure generated in the first 0.1 second of inspiratory occlusion (PO, l) is taken, which is a measure of the impulses or nerve discharges from the respiratory center and which is not affected by the mechanical properties of the lung or the cage thoracic.
The PO, 1 is. decreased by anesthetics and other respiratory center depressant drugs.
Ventilatory pattern. There are different pathological patterns:
Ataxic respiration: it is completely irregular and is observed in bulbar lesions.
Apneustic respiration: characterized by prolonged inspiratory pauses; seen in pons lesions.
Cheyne-Stokes respiration: it is the most frequently observed abnormal pattern and it occurs in cycles in which periods of apnea alternate with periods of increasing ventilation that then decreases until arriving again. to apnea.
Sleep study. Sleep has two phases separable with the electroencephalogram (EEG), the electromyogram (EMG) and the electrooculogram (EOG): REM sleep (rapid eye movements), characterized by generalized atony of the voluntary muscles except the extraocular ones, and the Non-REM sleep, which consists of four stages in which the waking low-voltage, fast-wave EEG activity gradually transforms into slow, high-voltage waves. Stages I and II of non-REM sleep are transitional between wakefulness and sleep, and stages III and IV are calm and stable sleep.
Normally in sleep all the components of ventilatory control are altered. Chemoreceptors sensitive to hypercapnia and hypoxemia decrease their activity by 50% in the non-REM stages and are inexplicable in REM. Central control becomes exclusively automatic and the effectors (respiratory muscles) are paralyzed except for the diaphragm. As a consequence of these changes, physiological apneas occur; during sleep, but in numbers less than 10 and with a duration of less than 10 seconds.
The most frequent and important respiratory disorders related to sleep are: obstructive apnea, central apnea, mixed apnea, obesity-hypoventilation syndrome, central alveolar hypoventilation syndrome, and sudden infant death syndrome.
Method. Polysomnography is a multidimensional system for the comprehensive evaluation of patients during sleep. Basically, it tries to determine the states of wakefulness, REM sleep and the different stages of non-REM sleep by means of the EEG, the EMG, and the EOG. At the same time, a group of physiological variables is measured: respiratory efforts, nasal and buccal air flow, arterial oxygenation, heart rate, intrathoracic pressure, etc.
Interpretation. In sleep apnea syndrome, the different types of apnea can be determined.
Obstructive apnea is diagnosed when there is no airflow in the nose and mouth and respiratory efforts persist or increase. In central apnea there is an absence of respiratory efforts and airflow. Mixed apnea. presents. characteristics: initial central apnea followed by obstruction.
Diffusion
The diffusion of oxygen has two limitations: one is the passage through the alveolocapillary membrane and the other is the binding of 02 to hemoglobin. Carbon monoxide (CO), which is commonly used to assess diffusion, binds rapidly to Hb and is therefore only limited by the alveolocapillary membrane.
CO diffusion capacity (DLco). Single breath method. It is measured by inhaling. give the patient a gaseous mixture with known concentrations of CO and an inert gas (helium or neon). The subject holds their breath for 10 seconds and exhales into a bag in order to quantify the drop in the concentration of CO and inert gas. This gas does not cross the alveolocapillary barrier but its concentration also decreases due to dilution in the residual volume, and it is used to correct the decrease in CO for the same reason. DLco is expressed in ml of diffused CO per mm Hg of concentration difference per minute (ml / mm Hg / minute).
DLco not only depends on the area and thickness of the membrane, but also other factors such as capillary blood volume; Hb concentration, ventilation homogeneity, and the presence of ventilation-perfusion irregularity, which is why this test is currently called CO transfer capacity.
Interpretation. The DLCo results are difficult to interpret and must be related to the values that correspond to the age, sex, height, body weight and Hb concentration of the examined patient.
DL is decreased in diffuse interstitial diseases even before clinical or radiological manifestations, in pulmonary emphysema, and in processes that somehow occupy the alveolar lumen; such as edema or pulmonary hemorrhage.
DLco is increased in exercise and in other situations where pulmonary blood flow has increased.
Exercise test. Is. The test is used to detect functional disorders that are not recognized at rest.
Method. A bicycle ergometer or treadmill is used with different workloads for the patient to make increasing efforts while many variables are measured: respiratory rate, total ventilation, tidal volume, heart rate, ECG, blood pressure, oxygen consumption , C02 removal, blood gases, diffusion capacity, etc.
Interpretation. The exercise test is usually diagnostic in cardiac ischemia and exercise-induced asthma.
In interstitial diseases with normal Pa02 at rest, exercise can trigger hypoxemia or exacerbated if previously had.
Normally, the 02 pressures equilibrate in 1/3 of the time that the alveolar air and capillary blood are in contact for exchange, when the subject is at rest (Fig. 22-1).
In patients with interstitial diseases and alterations in diffusion, the time required to balance the gases is longer and with exercise the blood flow is accelerated, the exchange time is shortened. and hypoxemia occurs.
Lung perfusion
Lung scan. The distribution of blood flow is measured fairly accurately using radioactive isotopes.
Method. It is injected. Albumin labeled usually with Tc 99 in a peripheral vein. The macroaggregates are trapped in the pulmonary capillaries distributed according to the blood flow and are recorded by an external radiation counter. In erect position. blood flow is maximum in the lung bases.
Lung scan is also used as a diagnostic guide in thromboembolism. The obstruction of a vessel is translated by a perfusion deficit, and when it is associated with an Xe scan without ventilation defects, it is suggestive of pulmonary thromboembolism.
Right catheterization. It is usually done with a balloon catheter (Swan-Ganz catheter) directed by blood flow.
Method. The catheter is placed through a vein (subclavian, jugular, brachial, femoral), passes through the right atrium and ventricle and its end is placed in the pulmonary artery.
Through this catheter, the pressures in the right atrium and the pulmonary artery and the pulmonary capillary pressure (which is similar to the pressure in the left atrium and the end-diastolic pressure of the left ventricle, in the absence of mitral valve disease) can be constantly measured .
Mixed venous blood is also drawn and cardiac minute volume can be measured by thermodilution technique or by applying the Fick principle. With all these data, the pulmonary and systemic vascular resistance are subsequently calculated.
Gas exchange function
The pulmonary gas exchange function. it is normal when arterial blood has approximately the same gas concentration as alveolar air, and arterial oxygen pressure (Pa02) and carbon dioxide (PaC02) are within normal values.
It is investigated by means of an arterial blood gas taken from a peripheral artery (radial, humeral, or femoral) in an anaerobic way and in a heparinized syringe so that the sample does not clot.
The most commonly used artery is the radial artery, but before puncturing it it is advisable to do the Allen test. The patient is asked to close the hand tightly, then the radial and ulnar arteries are simultaneously compressed, the latter is then decompressed, and the palm and fingers should regain their normal color. in 5 to 15 seconds. If it is longer than 15 seconds, this radial artery should not be punctured because in the event of thrombosis, the circulation from the ulnar could be insufficient and produce ischemia of the hand.
Once the sample is taken, the puncture site must be compressed for 3 to 5 minutes or more and the blood quickly sent to the laboratory for the determination of PaO2, PaCO2 and pH.
Interpretation. The normal value of Pa02 varies with age and is calculated by applying the following formula:
Pa02 = 109 - 0.43 X age.
The second step is to know the PAO2 by applying the alveolar gas equation:
PAO2 = Fi02x (PB-PvH2O) - PaCO2
0.8
where Fi02 (inspired fraction of O2) = 0.21 for ambient air; PB (atmospheric pressure) = 760 at sea level; and PvH2O (water vapor pressure) = 47.
Once the PA02 is calculated, it is subtracted. the Pa02 obtaining the gradient or alveolar-arterial difference of 02 (Aa D02) which is normal up to 15 mm Hg in young people and can reach up to 35 in the elderly.
The
decrease in Pa02 and the increase in Aa DO2 should suggest the two most frequent mechanisms of hypoxemia: ventilation-perfusion (VID.) Irregularity and intrapulmonary shunting. In practice, they are distinguished by making the patient inhale 100% O2; in areas of low (V / Q), but not short-circuited, increasing alveolar O2 corrects hypoxemia. If there is a short circuit (V / Q = O), the Pa02 is not modified.
The third cause of increased Aa DO} is the alteration of diffusion that does not allow the balance between alveolar and arterial O2, which occurs in rare cases, unless the transit time of the blood is shortened by the capillary, as occurs during fever, tachycardia or caused by exercise.
Hypoventilation is another cause of hypoxemia that must; suspected when PaC02 is increased but Aa DO2 is normal.
PaC02 is always analyzed together with pH because CO2 is related to metabolic state.
All metabolic alterations with modifications in blood bicarbonate produce immediate pulmonary ventilatory response ... to try to buffer the change in pH.
Example: If a patient has a metabolic acidosis with a bicarbonate concentration of 8 mEq / liter, the expected PaC02 for that state is 20 ± 2 mm Hg. If you have a metabolic alkalosis with a bicarbonate of 45 mEq / l, the lung will buffer the increase in pH and it may be that the expected PaC02 for that situation is 50 mmHg.
In the absence of acidosis or metabolic alkalosis, both the PaC02 of 20 and that of 50 mm Hg are abnormal and then one is in the presence of alkalosis and respiratory acidosis, respectively, which would trigger a renal compensatory response that is much slower than pulmonary (reaches equilibrium in 48 to 72 hours).
Importance of pulmonary functional assessment
The functional assessment is part of a routine sequence for the study of a wide variety of processes that affect the airways, lungs, rib cage, respiratory muscles, or the respiratory control system.
In choosing a certain functional test, it should be taken into account. the clinical case and the potential utility of the method to: quantify the functional deficit, follow the evolution of a disease, objectively assess the response to treatment, detect: subclinical alterations, and perform pre-occupational examinations and periodic controls in Occupational Medicine.
Of the tests developed in this chapter, forced spirometry, flow-volume curve, arterial blood gas, measurement of lung volumes, airway resistance, lung compliance, and diffusion capacity are commonly used. CO, and the exercise test. More and more attention is being paid to the assessment of respiratory muscles and the study of sleep.
In any case, there is no doubt that forced spirometry is the simplest and most widespread of the tests and that arterial blood gas is very important for the global assessment of pulmonary respiratory function.